Your Microbiome Holds the Key to Cancer Immunotherapy Success (Here’s What Science Just Found)
If you or someone you love is facing cancer, you’ve likely heard about “immunotherapy”—a revolutionary treatment that helps your own immune system fight tumors. But here’s the frustrating part: it doesn’t work for everyone. Why do some patients respond dramatically while others see no benefit?
A groundbreaking new meta-analysis of 71 clinical studies has uncovered a powerful, hidden predictor: your microbiome. That’s right—the trillions of bacteria and viruses living in and on your body aren’t just passive hitchhikers. They actively shape how well immunotherapy drugs, called immune checkpoint inhibitors (ICIs), work.
Let’s break down what this massive study found, in simple, actionable terms.
The Big Picture: Your Microbes Matter More Than You Think
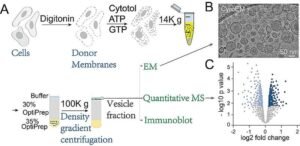
Researchers analyzed data from over 4,600 studies and zeroed in on 71 high-quality trials and cohort studies. Their goal? To see if the makeup of a patient’s microbiome (the community of microbes in their body) could predict whether immunotherapy would shrink their tumor or help them live longer.
The answer is a resounding yes.
The study looked at two main groups of microbes:
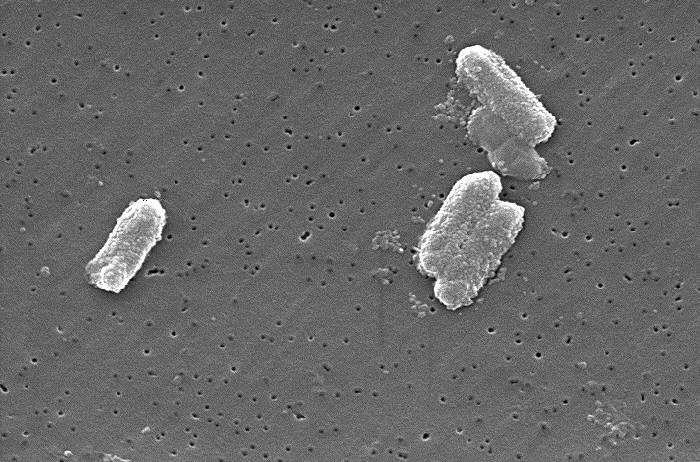
- Viruses (like Hepatitis B and HPV)
- Bacteria (the trillions in your gut and elsewhere)
And the results were striking: your microbial “fingerprint” can significantly influence your odds of responding to treatment.
Viruses: Not All Bad News for Cancer Patients
You might assume having a virus like Hepatitis B (HBV) or Human Papillomavirus (HPV) would make cancer treatment harder. Surprisingly, this study found the opposite for immunotherapy.
- Hepatitis B (HBV): Patients with HBV had a 36% higher chance of their tumor responding to immunotherapy (measured by Objective Response Rate, or ORR). This was especially true for liver cancer patients. Importantly, with proper antiviral medication, HBV reactivation during treatment was rare.
- HPV: Similarly, HPV-positive patients (often with head and neck cancers) had a 61% higher response rate to immunotherapy. Their tumors tend to be “hotter”—filled with immune cells ready to be unleashed by the drugs.
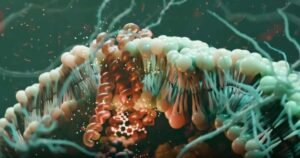
Why does this happen? It seems these viruses create a unique environment inside the tumor. They attract immune cells and “turn on” immune checkpoints like PD-1, making the tumor more visible and vulnerable to immunotherapy. It’s like the virus accidentally paints a target on the cancer for your immune system to hit.
The exception? Epstein-Barr Virus (EBV). In some cancers, like nasopharyngeal carcinoma, high EBV levels were linked to poorer responses. This highlights that not all viruses help—it depends on the type and the cancer.
Bacteria: It’s All About Balance and Location
While viruses showed a clearer link to initial tumor response, bacteria were more strongly tied to long-term survival (Overall Survival and Progression-Free Survival).
- Diversity is Key: Patients with a richer, more diverse gut microbiome tended to live longer without their cancer progressing. One analysis showed high diversity was linked to a 36% lower risk of cancer worsening.
- Location, Location, Location: The study found that microbes living inside the tumor itself might be even more important than those in the gut. Bacteria like Streptococcus found within tumors were linked to better responses, likely because they help immune cells recognize and attack the cancer.
- Cancer-Specific Effects:
- Liver & Lung Cancer: Having the “right” bacteria was linked to significantly better survival.
- Gastrointestinal Cancers: Surprisingly, certain bacteria (like H. pylori, a known stomach cancer trigger) were linked to worse outcomes with immunotherapy. This suggests the relationship is complex and depends heavily on the cancer type.
The Power of Teams: Why Microbial Communities Beat Solo Players
One of the most exciting findings? Combinations of microbes are better predictors than single species.
Think of your microbiome as a soccer team. One star player (like Bifidobacterium) might help, but it’s the coordinated play of the entire team that wins the game. The study found that models looking at multiple bacterial species together were much better at predicting who would benefit from immunotherapy than models looking at just one.
This is why simply taking a probiotic with one “good” bacterium probably isn’t enough. Future treatments might involve transplanting an entire healthy microbial community (fecal microbiota transplantation, or FMT) from a responder to a non-responder—and early trials show this can indeed boost response rates.
What About Side Effects? The Safety Question
Immunotherapy can cause serious side effects, often because it revs up the immune system too much. The study looked at whether your microbiome predicts these risks.
The good news? Overall, having a virus like HBV or HPV did not increase the general risk of side effects.
The nuanced news? In liver cancer patients, having HBV was actually linked to a lower risk of severe side effects. However, in patients getting single-drug immunotherapy (monotherapy), viral infections were linked to a higher risk of serious adverse events. This suggests the interaction is complex and needs more study.
What This Means for You: The Future of Personalized Cancer Care
This research is a giant leap toward truly personalized cancer medicine. Here’s what it could mean:
- Microbiome Testing Before Treatment: In the future, a simple stool test or even a tumor biopsy could be used to analyze your microbiome. This would help doctors predict if immunotherapy is your best bet—or if you might need a different approach.
- Microbiome Modulation: If your microbiome isn’t ideal, doctors might try to change it before starting immunotherapy. This could involve:
- Fecal Microbiota Transplantation (FMT): Transplanting stool (and its microbes) from a patient who responded well to immunotherapy.
- Precision Probiotics/Prebiotics: Tailored supplements to encourage the growth of beneficial microbes.
- Dietary Changes: Food directly feeds your gut bacteria. A microbiome-friendly diet could become part of cancer treatment.
- Avoiding Microbiome Killers: The study reinforces that antibiotics, which wipe out gut bacteria, can hurt immunotherapy outcomes. Doctors may become much more cautious about prescribing them during treatment.
The Bottom Line: Your Bugs Are Part of Your Cancer Fight
This massive analysis confirms what many scientists have suspected: your microbiome is not a bystander in cancer treatment—it’s an active player. Viruses like HBV and HPV, and a diverse community of gut and tumor bacteria, can significantly boost your chances of beating cancer with immunotherapy.
While we’re not yet at the point of routine microbiome testing for every cancer patient, this research paves the way. It tells us that nurturing your inner ecosystem might be just as important as the drugs you take.
If you’re considering immunotherapy, talk to your oncologist about the latest research on the microbiome. The future of cancer care is looking more personalized—and more microbial—than ever.






Post Comment