Unveiling the Intricacies of Microbial Pathogenesis: Understanding How Microorganisms Cause Disease in Humans
Introduction:
 Microbial pathogenesis is a multifaceted process whereby microorganisms, including bacteria, viruses, fungi, and parasites, employ an array of strategies to colonize, evade host defenses, and ultimately cause disease in humans. This article delves into the intricate mechanisms underlying microbial pathogenesis, encompassing virulence factors, host-pathogen interactions, and immune responses.
Microbial pathogenesis is a multifaceted process whereby microorganisms, including bacteria, viruses, fungi, and parasites, employ an array of strategies to colonize, evade host defenses, and ultimately cause disease in humans. This article delves into the intricate mechanisms underlying microbial pathogenesis, encompassing virulence factors, host-pathogen interactions, and immune responses.
Virulence Factors:
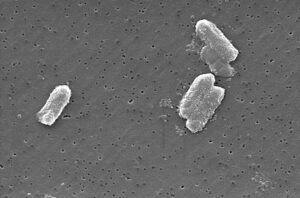
 Virulence factors are molecular components produced by pathogens that contribute to their ability to cause disease. Bacteria may produce toxins, such as exotoxins and endotoxins, which disrupt host cell function or elicit harmful immune responses. Examples include the potent cytotoxins produced by Clostridium difficile and the lipopolysaccharide endotoxin of Gram-negative bacteria. Additionally, bacterial pathogens may possess adhesion molecules that facilitate attachment to host cells or tissues, enhancing their ability to colonize and invade.
Virulence factors are molecular components produced by pathogens that contribute to their ability to cause disease. Bacteria may produce toxins, such as exotoxins and endotoxins, which disrupt host cell function or elicit harmful immune responses. Examples include the potent cytotoxins produced by Clostridium difficile and the lipopolysaccharide endotoxin of Gram-negative bacteria. Additionally, bacterial pathogens may possess adhesion molecules that facilitate attachment to host cells or tissues, enhancing their ability to colonize and invade.
Similarly, viruses utilize various virulence factors to subvert host defenses and propagate within the host. These may include viral surface proteins that mediate attachment and entry into host cells, as well as proteins that interfere with host immune responses or promote viral replication. For instance, the hemagglutinin and neuraminidase proteins of influenza virus play pivotal roles in viral attachment and release, respectively.
Fungal and parasitic pathogens also deploy an assortment of virulence factors to establish infection and cause disease. Fungi may produce toxins, enzymes, or cell wall components that facilitate tissue invasion and evasion of host immune defenses. Parasites, such as Plasmodium spp. (malaria parasites) and Trypanosoma cruzi (causative agent of Chagas disease), possess complex life cycles and mechanisms for evading host immune responses, allowing them to persist and cause chronic infections.
Host-Pathogen Interactions:
Successful microbial pathogenesis relies on intricate interactions between pathogens and their human hosts. Pathogens must overcome physical barriers, evade innate immune defenses, and exploit host cellular processes to establish infection. Adherence to host cells or tissues is often the first step in the pathogenic process, facilitated by microbial adhesins and host cell receptors. Once attached, pathogens may secrete enzymes or toxins to breach epithelial barriers and gain access to deeper tissues.
Upon encountering pathogens, the host immune system mounts a coordinated response aimed at eliminating the invaders. Innate immune cells, such as macrophages and neutrophils, recognize conserved microbial components known as pathogen-associated molecular patterns (PAMPs) via pattern recognition receptors (PRRs), triggering inflammatory responses and antimicrobial activities. Meanwhile, adaptive immune responses, mediated by T and B lymphocytes, provide antigen-specific defense mechanisms that confer long-term immunity.
Immune Responses:
Microbial pathogens have evolved diverse strategies to evade or subvert host immune responses, enabling them to persist within the host and cause disease. Some pathogens evade immune surveillance by modulating their surface antigens to evade recognition by host antibodies or by suppressing host immune cell function. For example, Mycobacterium tuberculosis can survive and replicate within host macrophages by inhibiting phagosome-lysosome fusion and antigen presentation.
In other cases, pathogens may actively manipulate host immune signaling pathways to their advantage. Certain viruses encode proteins that interfere with cytokine signaling or inhibit apoptosis, allowing them to evade host immune surveillance and establish persistent infections. Similarly, parasitic pathogens may induce immunomodulatory responses in the host, such as the polarization of T cell responses towards a Th2 phenotype, which promotes parasite survival and proliferation.
Conclusion:
In summary, the pathogenesis of microbial infections involves a complex interplay between virulence factors, host-pathogen interactions, and immune responses. Understanding these mechanisms is crucial for developing strategies to prevent and treat infectious diseases. By elucidating the molecular basis of microbial pathogenesis, researchers can identify novel targets for antimicrobial therapy and vaccine development, ultimately advancing our ability to combat infectious diseases and safeguard public health.








Post Comment