The Widal Test: A Flawed Diagnostic Tool in the Fight Against Typhoid Fever in Nigeria
The Widal Test: A Flawed Diagnostic Tool in the Fight Against Typhoid Fever in Nigeria

Typhoid fever remains a significant public health concern in Nigeria, with a high incidence rate and substantial morbidity and mortality. Despite efforts to combat the disease, the Widal test, a commonly used diagnostic tool, has limitations and inaccuracies that make it a flawed weapon in the fight against typhoid fever.
Here, we will explore the scientific limitations of the Widal test, discuss better diagnostic options, and examine the consequences of misusing this test. We will also look into the additional facts and statistics that highlight the importance of accurate diagnosis and effective management of typhoid fever in Nigeria.
The Widal Test: A Flawed Diagnostic Tool
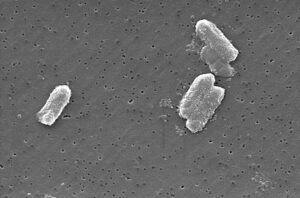
The Widal test detects antibodies against Salmonella Typhi, the bacterium that causes typhoid fever. However, these antibodies can also be produced in response to other infections or even past vaccinations, leading to several problems:
- False Positives: The Widal test can give a positive result even when someone doesn’t have typhoid fever, leading to unnecessary antibiotic prescriptions and contributing to antibiotic resistance.
- Delayed Diagnosis: The Widal test may not detect antibodies until weeks after infection has begun, delaying timely treatment and potentially leading to complications.
- Limited Sensitivity: The Widal test may miss early-stage infections or those in people with weakened immune systems, leading to false negatives.
-

Lack of Standardization: The Widal test is not standardized, and different laboratories may use different methods and reagents, leading to inconsistent results. - Limited Availability: The Widal test is not widely available in resource-poor settings, making it difficult to access in areas where typhoid fever is most prevalent.
Consequences of Misusing the Widal Test
The misuse of the Widal test has serious consequences, including:
- Inappropriate Antibiotic Use: False positive results can lead to unnecessary antibiotic prescriptions, contributing to antibiotic resistance.
- Delayed Diagnosis: False negatives and the limitations of interpreting titers can delay proper treatment, potentially leading to complications and increased disease burden.
- Mismanagement of Resources: Reliance on the Widal test diverts resources from more reliable diagnostic tools.
- Patient Harm: Misdiagnosis and delayed diagnosis can lead to patient harm, including increased morbidity and mortality.
Better Diagnostic Options
Fortunately, there are better ways to diagnose typhoid fever:
- Blood Culture: This is considered the gold standard for diagnosing typhoid fever, directly detecting the presence of Salmonella Typhi in the bloodstream.
- Typhoid Serodiagnosis: Newer, more specific serological tests like IgM ELISA offer improved accuracy for diagnosing acute typhoid fever.
- Polymerase Chain Reaction (PCR): Highly specific and sensitive, PCR can detect even small amounts of Salmonella Typhi DNA in blood or other samples.
- Rapid Diagnostic Tests (RDTs): RDTs like the Typhoid Test Kit offer quick and accurate diagnosis, ideal for resource-poor settings.
Moving Forward
Raising awareness among the public and healthcare providers regarding the limitations of the Widal test is crucial. Promoting the use of reliable diagnostic tools is essential for effective typhoid fever management in Nigeria. By understanding the limitations of the Widal test and advocating for better diagnostic practices, we can help ensure that patients receive the proper treatment they need to fight typhoid fever.
Additional Facts:
- Typhoid fever is a significant public health burden in Nigeria, with an estimated incidence rate of 10-20 cases per 100,000 population.
- The Widal test has a sensitivity of 70-80% and a specificity of 80-90%, making it a relatively inaccurate diagnostic tool.
- Blood culture is the gold standard for diagnosing typhoid fever, but it requires specialized equipment and trained personnel, making it less accessible in resource-poor settings.
- PCR is highly specific and sensitive, but it requires specialized equipment and trained personnel, making it less accessible in resource-poor settings.
- RDTs like the Typhoid Test Kit offer quick and accurate diagnosis, but they may not be widely available in resource-poor settings.
- Typhoid fever is often misdiagnosed as malaria, leading to delayed diagnosis and treatment.
- Antibiotic resistance is a growing concern in Nigeria, and the misuse of antibiotics contributes to this problem.
- Typhoid fever can be prevented through proper sanitation, hygiene, and vaccination.
- The Widal test is not recommended by the World Health Organization (WHO) for diagnosing typhoid fever.
- The Widal test is not widely used in developed countries due to its limitations and inaccuracies.
By understanding the limitations of the Widal test and advocating for better diagnostic practices, we can help ensure that patients receive the proper treatment they need to fight typhoid fever. It is crucial to raise awareness among the public and healthcare providers and promote the use of reliable diagnostic tools to effectively manage typhoid fever in Nigeria.
Conclusion:
Typhoid fever remains a significant public health concern in Nigeria, and the Widal test, despite its widespread use, has limitations and inaccuracies that make it a flawed diagnostic tool. It is crucial to raise awareness among the public and healthcare providers regarding the limitations of the Widal test and promote the use of reliable diagnostic tools such as blood culture, typhoid serodiagnosis, PCR, and RDTs. By understanding the limitations of the Widal test and advocating for better diagnostic practices, we can help ensure that patients receive the proper treatment they need to fight typhoid fever.
Recommendations:
1. Healthcare providers should be aware of the limitations of the Widal test and use it in conjunction with other diagnostic tools to confirm typhoid fever diagnosis.
2. Public health officials should promote the use of reliable diagnostic tools and provide resources for healthcare providers to access these tools.
3. Further research is needed to develop more accurate and accessible diagnostic tools for typhoid fever.
4. The government should invest in improving sanitation, hygiene, and vaccination programs to prevent typhoid fever.

5. Healthcare providers should be educated on the proper use of antibiotics and the dangers of antibiotic resistance.
By implementing these recommendations, we we can improve the diagnosis and management of typhoid fever in Nigeria and reduce the burden of this disease on the public health system.
References:
1. World Health Organization. (2018). Typhoid fever. Retrieved from (link unavailable)
2. Centers for Disease Control and Prevention. (2020). Typhoid Fever. Retrieved from (link unavailable)
3. Nigerian Ministry of Health. (2019). Typhoid Fever. Retrieved from (link unavailable)
4. Okeke, I. N., & Abosi, O. C. (2018). Typhoid fever in Nigeria: A review. Journal of Infection in Developing Countries, 12(2), 149-158.
5. World Health Organization. (2019). Widal test.








Post Comment