The Art of Deception: How Parasites Evade the Human Immune System
The Art of Deception: How Parasites Evade the Human Immune System
Introduction
Man’s relationship with parasites is remarkably interesting and seems to have evolved over time with both man and parasite evolving to the current state. Parasitic infections worldwide constitute a fifth of all infectious diseases. The burden is however highest in the developing world and particularly so in the immunocompromised where Toxoplasma gondii and Cryptosporidium are of particular concern. It is estimated that there is about 45% co-infection rate with T. gondii and HIV in sub-Saharan Africa.1
 While various relationships such as mutualism and commensalism exist between man and microbes, parasitism is a condition in which only the host derives all the benefits. In order to derive these benefits, the parasites must spend adequate time within the host, develop, replicate and then be transmitted to the vector for further propagation of the life cycle of the species.
While various relationships such as mutualism and commensalism exist between man and microbes, parasitism is a condition in which only the host derives all the benefits. In order to derive these benefits, the parasites must spend adequate time within the host, develop, replicate and then be transmitted to the vector for further propagation of the life cycle of the species.
Classification of parasites
Taxonomy of parasites follows phylum, class, order, suborder, super family, family, subfamily, genus, species and subspecies. Some of these are omitted for certain parasites. Parasites may be divided into endoparasites which reside within the host; and ectoparasites which reside outside the host. Of the endoparasites are protozoa and metazoa. The subkingdom Protozoa comprises the simple single-celled eukaryotes with intracellular organelles which are membrane-bound, and they commonly show the characteristics of living things. These parasites are subdivided into seven phyla of which Sarcomastigophora), Apicomplexa, Ciliophora and Microsporidia are medically significant.2 These classifications are based on the parasites’ motility and cell structure.
- Amoeba (Sarcodina) move via pseudopods and digest food via phagocytosis e.g., Entamoeba histolytica, Balamuthia madrillaris, Naegleria fowleri.

- Flagellates (Mastigophora) move with the aid of their flagella e.g., Giardia duodenalis, Trypanosoma cruzi, Leishmania donovani.
 Apicomplexa (Sporozoa) have an apical complex. Some of the stages of these parasitic protozoa are motile such as the ookinete in Plasmodium life cycle while others are non-motile such as the oocyst stage. Examples of members of this class are: Plasmodium falciparum, Toxoplasma gondii, Cryptosporidium parvum.
Apicomplexa (Sporozoa) have an apical complex. Some of the stages of these parasitic protozoa are motile such as the ookinete in Plasmodium life cycle while others are non-motile such as the oocyst stage. Examples of members of this class are: Plasmodium falciparum, Toxoplasma gondii, Cryptosporidium parvum.  Ciliates (Ciliophora) move with the aid of cilia which cover the entire circumference of the organism. The only medically important ciliate is Balantidium coli.
Ciliates (Ciliophora) move with the aid of cilia which cover the entire circumference of the organism. The only medically important ciliate is Balantidium coli.- Microsporidia (Microsporida) tiny intracellular organisms that produce spores containing a characteristic coiled polar tube. A common one is Cystoisospora beli.
Despite the variation in their life cycles, majority of the protozoa propagate by simple asexual cell division of the motile feeding trophozoite stage; many undergo formation of a non-motile encysted stage, while others have an asexual and sexual phase.
Metazoa consist of the nemathelminths and Platyhelminthes also referred to as round and flat worms, respectively.
The Platyhelminthes are further subdivided into cestodes and trematodes.
Nemathelminths (nematodes)
- Cylindrical worms with shiny cuticle
- Simple digestive system
- Separate sexes
- Nematodes, which infect humans, live in the tissues or intestinal tract. Transmission is usually via insect vectors (tissue nematodes) or from faeco-oral routes.
Cestodes (tape worms)
- Possess a tape-like body with head (scolex) and proglottids. The head attaches the tapeworm to its host by suckers and in some species hooks also.
 Tape worms are hermaphroditic with male and female reproductive organs being found in each mature proglottid.
Tape worms are hermaphroditic with male and female reproductive organs being found in each mature proglottid.- Nutrition is via body surface penetration
Trematodes (flukes)
- Unsegmented, mostly flat leaf-like worms (except schistosomes)
 Attach to their host by means of oral and ventral suckers and they lack a body cavity
Attach to their host by means of oral and ventral suckers and they lack a body cavity- All trematodes are hermaphroditic (except schistosomes).
- Most trematodes eggs are operculated (with lids).
Evasion strategies
The human body is an amazing machine with an armamentarium developed to prevent invasion by parasites seeking to disturb its homeostasis. There is a subtle interplay between the host defence mechanisms and survival strategies of the parasite. For any infection to occur, the host must be susceptible, and the parasite needs the ability to penetrate and survive in the host.
On contact with the human body, parasites must first conquer the innate barrier of the skin, gastrointestinal tract and other portal of entry in order to gain access into the plentiful supply of nutrients within the host. This first line of defence includes mechanisms such as the epithelial barrier, mast, dendritic and natural killer cells, eosinophils, macrophages, complement activation with opsonisation etc. Following evasion of these intrinsic immune mechanisms, these organisms must then encounter the adaptive immunity machinery which seek to end the sojourn of the parasites into their territory. These mechanisms include the activities of the cell-mediated and humoral adaptive immunity with delayed type hypersensitivity, antibody and granuloma formation and antibody-dependent cell-mediated cytotoxicity (ADCC).3
Only parasites which have successfully adapted to eluding both the innate and acquired immunity can survive in vivo. For these parasites to survive in the human body, they have also evolved a multitude of mechanisms. These mechanisms vary from mere camouflage with the host proteins to complex measures such as antigenic variation. Immune evasion was discovered a century ago by Paul Ehrlich.4 An African proverb states that ‘Once the hunter learns to shoot without missing, the bird must learn to fly without perching’. This leads us to how these endoparasites have evolved to ‘flying without perching’ to evade man’s immune response mechanisms aimed at truncating their survival in vivo.

Protozoa
One of the striking features of protozoa is their tissue specificity. Some mechanisms protozoa deploy to evade host immunity include:
- Antigenic masking: Parasites become coated with host components hence are not recognised as foreign to the patrolling immune cells5.
- Plasmodium spp. For example, can sequester themselves in hepatocytes or hepatocyte derived membrane vacuoles. They are unrecognized as they seem to be hepatocytes5,6
- Trypanosomes, Toxoplasma and Leishmania spp. also deploy this mechanism and hide out within red blood cells and macrophages in order to transit freely through the blood stream and avoid destruction5,7.
- Knob-associated histidine-rich protein present on the surfaces of erythrocytes infected with Plasmodium are involved in displaying PfEMP1 proteins which mediate cellular adhesion and retard their progress to the spleen hence allowing parasites to become sequestered in tissues.8
- Anatomic seclusion: The strategy here is to hide in host tissues and organs to escape cells of the immune system.
- This is typical of Toxoplasma gondii infection where it reaches host sites with limited immune cells such as central nervous system where they usually initiate low-grade infection.9
- Merosomes budded off from hepatocyte membranes and contain merozoites; this membrane enables plasmodia to escape phagocytosis by macrophages and Kupffer cells of the liver. These merosomes lack signals that trigger macrophages such as phosphatidyl-serine flipping of the cell membrane hence subvert engulfment14,15.
- Sequestration of hypnozoites in the hepatocytes may lead to recurrence of malaria symptoms referred to as relapse. This occurs in P. ovale and P. vivax. After completion of antimalarial medications, these metabolically-inert persister cells may resurface however, the mechanisms involved in this immune evasion are poorly understood.17
- Toxoplasma spp have ability to survive intracellular like because they have processes for transmembrane transport of nutrients.
- Antigenic variation: Protozoa consist of different stages of development. These parasites exhibit a diverse group of proteins which they elaborate on their surfaces and change continuously during the stages of their life cycles which confuse the patrolling antigen presenting cells.
- The presence of gene cassettes seen in Trypanosoma brucei gambiense facilitate switching to different variant surface glycoproteins (VSG) in a bid to dodge being recognised by the immune surveillance cells. This allows the Trypanosoma spp. evade antibody detection, reproduction and maintain persistent infection.9
- The circumsporozoite (CS protein) on P. falciparum sporozoite surface coat has a long series of tandem repeats of amino acids resulting in a genome with rapidly changing sequences as well as changes in protein activity causing phenotypic changes aiding its adaptation.8
- P. falciparum sporozoite surface coat has a long series of tandem repeats of amino acids resulting in a genome with rapidly changing sequences as well as changes in protein activity causing phenotypic changes aiding its adaptation. Those antigens which undergo the most variation are those selected for expression on red blood cells. Examples are antigens encoded by var genes, and the Plasmodium interspersed repeats (pir) genes6,16.
- A different strategy of antigenic variation is employed by plasmodia. During pre-erythrocytic schizogony develop mutations during repeated cycles of replication. This results in numerous clones of parasite which the body’s memory cells may not be able to recall and mount an appropriate response against. These polymorphisms may affect the efficacy of vaccines developed against malaria6,16.
- Encystment: Cyst forms are more resistant to environmental conditions than un-cysted forms of parasites. The casing serves as a form of armour.
- Entamoeba histolytica is an infective cyst that excysts in the colon after evading the acidic pH of the stomach. The hardy cyst can survive the acidic stomach and pass through.
- Immune suppression of host: Some protozoa may induce immunosuppression in the host. This is a mechanism to escape immune surveillance. Protozoa accomplish this by excretion of regulatory cytokines to stimulate the proliferation of suppressor T-cells that inhibit the immune system; and by producing specific immune suppressor substances5.
- Leishmania spp are able to increase IL-10 (immunosuppressive in action) which causes reduced production of the proinflammatory cytokines, IL-12, and TNF-α in macrophages.9 Some parasites such as Leishmania are known to use host cytokines as growth factors while some cestodes use antibodies as nutrients10.
- The engulfment of the malaria pigment by the circulating macrophages weakens their phagocytic ability. Hemozoin-laden macrophages have diminished ability to generate free radicals adversely affecting their immunologic function14,17.
- Anti-immune machinery:
- Leishmania spp. produce antioxidants to counter the oxidative burst of macrophages. This protozoa also inactivates complement factor C3b which facilitates complement mediated phagocytosis – hence opsonization and consequent phagocytosis does not occur11.
- Brugia malayi produces a serpin (Bm-SNP-2) that targets and inhibits neutrophil-secreted cathepsin G and elastases.
- Entamoeba histolytica can induce neutrophil apoptosis and suppress macrophage production of nitric oxide9.
- Dendritic cells development and immunologic responses are retarded in the presence of PfEMP-1-expressing malaria parasites diminishing their ability to prime T cell responses through production of cytokines such as interleukin-12. Conversely, there is elevated interleukin 10 activity which has the ability to suppress inflammation.14,15
- Following the release merozoites to attack the red blood cells, the action of complement is evaded by the binding of infected erythrocytes to a complement regulatory factor- factor H, thwarting the formation of the membrane attack complex (MAC) which would ordinarily culminate in cellular lysis.14
- Tissue invasion:
- Hepatocyte invasion is mediated by the CS protein of Plasmodium spp plays a critical role in the invasion by sporozoites of hepatocytes8,12.
- Invasion and seclusion in erythrocytes are also an immune escape mechanism for plasmodia. Merozoite surface protein (MSP) 1 facilitates attachment and consequent entry to erythrocytes6.
- Leishmania promastigotes secrete a metalloprotease (leishmanolysin) which functions to digest extracellular matrix proteins and open a pathway for invasion11.
- Decoy mechanisms
- PfEMP1 proteins – of the var gene family – bind to erythrocytes through complement receptor 1 to form rosettes facilitating sequestration while circumventing splenic elimination.7,14
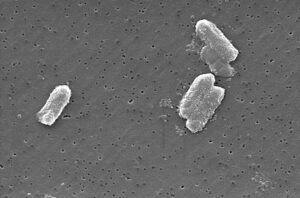
Metazoa
The metazoan parasites include the round and flat worms classified as nemathelminths and Platyhelminthes, respectively. These are masters at manipulating the host immune defences as they would be rapidly detected by the host’s immune system were it not for their ability to prolong their survival in the human body by the following mechanisms:
- Large size: The large size of helminths enables them to resist engulfment by the macrophages. Their sheer size makes parasite elimination difficult.
- Antigenic masking: This mechanism for evasion employed by both protozoa and helminths. Erythrocyte antigens on the tegument of cestodes and trematodes help the worms to be seen as self. Schistosoma coat themselves with blood group antigens and MHC classes I and II such that they cannot be detected as non-self.
- Molecular mimicry of host structure: Schistosomes produce schistosome complement inhibitor (SCIP-1) which is antigenically like some human complement inhibitors such as CD59. Thus, SCIP-1 acts like CD59 to bind C8 and C9 and block MAC18.
- Anatomic seclusion:
- Cysts of Taenia spp. could lead to cysticercosis on invasion of sites with few immune cells such as the central nervous system or the eye10.
- S. haematobium reside in the vesical plexus surrounding the bladder where the female lays ova which penetrate the bladder submucosa with its lateral spine and exits to be excreted via urine into water bodies to continue its life cycle.
- Trichinella spiralis larva is also excellent at sequestrating itself in poorly patrolled mammalian muscle cells.10
- Surface shedding: Toxocara canis larvae were demonstrated to exhibit this property of shrugging off their outer coat with surface-bound antibodies19.
- Immune suppression of host:
- Components from helminths such as B. malayi and trematodes such as Fasciola hepatica produce TGFβ homologs effectively stimulating regulatory T and B cells and inducing tolerance20.
- Eosinophil apoptosis can be induced by Paragonimus-derived products such as excretory-secreted products (ESP) via caspase 3 activation21.
- Anti-immune mechanisms:
- Liver fluke larvae produce antioxidases e.g., glutathione peroxidase and superoxide dismutase to neutralize nitric oxide produced by neutrophils and macrophages to destroy as seen in which produce enzymes that cleave antibodies.
- Echinococcus granulosus possesses antigen B which suppresses dendritic cell development and monocyte differentiation with resultant diminished host immune response to its presence20.
- Ova of Schistosoma mansoni produce bioactive antigens like lysophosphatidylserine which mitigate inflammatory responses by targeting toll-like receptors20.
- The filarial worm, Brugia malayi secretes abundant larval transcript (ALT-2). This downregulates IFN-dependent signals.20
- Migration: Continuous motion prevents the resident macrophages from neutralising parasites.
- Schistosoma haematobium larvae migrate from lungs to heart via pulmonary veins then to portal veins and liver.
- Taenia spp. also migrate from the duodenum to the intestinal wall with the help of their hooks to enter the venous blood stream. Here, the larvae are carried until they reach the skeletal muscles where they become cysticerci.
- Encystation: The metacercariae of P. westermani excyst in the hostile acidic conditions of the stomach and penetrate the intestinal wall to migrate to the lungs via the peritoneal and pleural cavities in order to propagate their lifecycle.
Table1: Summary of strategies deployed by various pathogens
| IMMUNE STRATEGIES | PATHOGENS | |
| PROTOZOA | Antigenic masking | Plasmodium spp., Toxoplasma gondii, Leishmania spp. |
| Anatomic seclusion | Toxoplasma gondii, Plasmodium spp. | |
| Antigenic variation | Trypanosoma spp., Plasmodium spp. | |
| Encystation | Entamoeba histolytica | |
| Immunomodulation | Leishmania spp., Entamoeba histolytica, Ascaris lumbricoides | |
| Anti-immune machinery | Leishmania spp., Brugia malayi | |
| Tissue invasion | Plasmodium spp, Leishmania spp. | |
| METAZOA | Large size | Schistosoma spp.,
Ascaris lumbricoides |
| Antigenic masking | Schistosoma spp., Echinococcus granulosus | |
| Molecular mimicry | Schistosoma spp. | |
| Anatomic seclusion | Taenia spp., Trichinella spiralis | |
| Immune suppression | Brugia malayi, Fasciola hepatica, Paragonimus westermani | |
| Anti-immune mechanisms | Echinococcus granulosus, Schistosoma mansoni, Brugia malayi | |
| Migration | Schistosoma haematobium, Taenia spp. | |
| Encystation | Paragonimus westermani |
Conclusion
There is a myriad of mechanisms by which eukaryotic parasites manipulate the immune system in order to perpetuate their lifestyle and these manoeuvres can be harnessed in order to create targets for medications or vaccines in future.
References
1. Wang Z, Wang S, Liu H, et al. Prevalence and burden of Toxoplasma gondii infection in HIV-infected people : a systematic review and meta-analysis. Lancet HIV. 4(4):e177-e188. doi:10.1016/S2352-3018(17)30005-X
2. Levine ND, Corliss JO, Cox FEG, et al. A Newly Revised Classification of the Protozoa. J Protozool. 1980;27(1):37-58. doi:10.1111/j.1550-7408.1980.tb04228.x
3. Delves PJ, Martin SJ, Burton DR, Roitt IM. Roitt’s Essential Immunology. 13th ed. West Sussex, UK: Wiley-Blackwell; 2017.
4. Schmid-Hempel P. Parasite immune evasion: a momentous molecular war. Trends Ecol Evol. 2008;23(6):318-326. doi:10.1016/j.tree.2008.02.011
5. Seed JR. Protozoa: Pathogenesis and Defenses. University of Texas Medical Branch at Galveston; 1996.
6. Belachew EB. Immune Response and Evasion Mechanisms of Plasmodium falciparum Parasites. J Immunol Res. 2018;2018. doi:10.1155/2018/6529681
7. Olivier M, Gregory DJ, Forget G. Subversion mechanisms by which Leishmania parasites can escape the host immune response: A signaling point of view. Clin Microbiol Rev. 2005;18(2):293-305. doi:10.1128/CMR.18.2.293-305.2005
8. Davies HM, Nofal SD, McLaughlin EJ, Osborne AR. Repetitive sequences in malaria parasite proteins. FEMS Microbiol Rev. 2017;41(6):923-940. doi:10.1093/femsre/fux046
9. Morrot A, Marriott I. Editorial: Immune Evasion Strategies in Protozoan-Host Interactions. Article. 2020;11:1. doi:10.3389/fimmu.2020.609166
10. Schmid-Hempel P. Immune defence, parasite evasion strategies and their relevance for “macroscopic phenomena” such as virulence. Philos Trans R Soc B Biol Sci. 2009;364(1513):85-98. doi:10.1098/rstb.2008.0157
11. Teixeira JE, Sateriale A, Bessoff KE, Huston CD. Control of Entamoeba histolytica adherence involves metallosurface protease 1, an M8 family surface metalloprotease with homology to leishmanolysin. Infect Immun. 2012;80(6):2165-2176. doi:10.1128/IAI.06389-11
12. Zhao J, Bhanot P, Hu J, Wang Q. A comprehensive analysis of Plasmodium circumsporozoite protein binding to hepatocytes. PLoS One. 2016;11(8). doi:10.1371/journal.pone.0161607
13. Hartmeyer GN, Stensvold CR, Fabricius T, et al. Plasmodium cynomolgi as Cause of Malaria in Tourist to Southeast Asia, 2018. Emerg Infect Dis. 2019;25(10):1936-1939. doi:10.3201/eid2510.190448
14. Rénia L, Goh YS. Malaria parasites: The great escape. Front Immunol. 2016;7(Nov):1-14. doi:10.3389/fimmu.2016.00463
15. Zheng H, Tan Z, Xu W. Immune Evasion Strategies of Pre-Erythrocytic Malaria Parasites. Mediators Inflamm. 2014;2014:1-6. doi:10.1155/2014/362605
16. Morrot A. Editorial: Immune Evasion Strategies in Protozoan-Host Interactions. Front Immunol. 2020;11:8-10. doi: 10.3389/978-2-88966-294-4
17. Gomes PS, Bhardwaj J, Rivera-Correa J, Freire-De-Lima CG, Morrot A. Immune escape strategies of malaria parasites. Front Microbiol. 2016;7(OCT). doi:10.3389/fmicb.2016.01617
18. Fishelson Z. Novel mechanisms of immune evasion by Schistosoma mansoni. Mem Inst Oswald Cruz. 1995;90(2):289-292. doi:10.1590/S0074-02761995000200029
19. Blaxter ML, Rudin W, Maizels RM. Nematode Surface Coats: Actively Evading Immunity. Parasitol Today. 1992;8(7):243-247.
20. Zakeri A, Hansen EP, Andersen SD, Williams AR, Nejsum P. Immunomodulation by helminths: Intracellular pathways and extracellular vesicles. Front Immunol. 2018;9(OCT). doi:10.3389/fimmu.2018.02349
21. Min DY, Lee YA, Ryu JS, et al. Caspase-3-mediated apoptosis of human eosinophils by the tissue-invading helminth Paragonimus westermani. Int Arch Allergy Immunol. 2004;133(4):357-364. doi:10.1159/000077355









Post Comment