Stains in Microbiology: The Essential Guide to Identifying Bacteria, Fungi, and More
Stains in Microbiology: How Coloring Cells Reveals the Invisible World of Pathogens
Microorganisms are everywhere—on your skin, in your gut, in the air you breathe. But most are invisible to the naked eye, and even under a microscope, they’re nearly transparent. So how do scientists “see” them clearly enough to identify, classify, and treat the ones that cause disease?
The answer lies in one of microbiology’s oldest—and most powerful—tools: staining.
Staining isn’t just about adding color. It’s a strategic chemical process that highlights cellular structures, reveals differences between microbes, and guides clinical decisions. From the classic Gram stain to advanced fluorescent techniques, staining remains indispensable in labs worldwide.
Let’s explore the major types of stains, how they work, and why they matter in clinical practice.
Why Staining Is Necessary
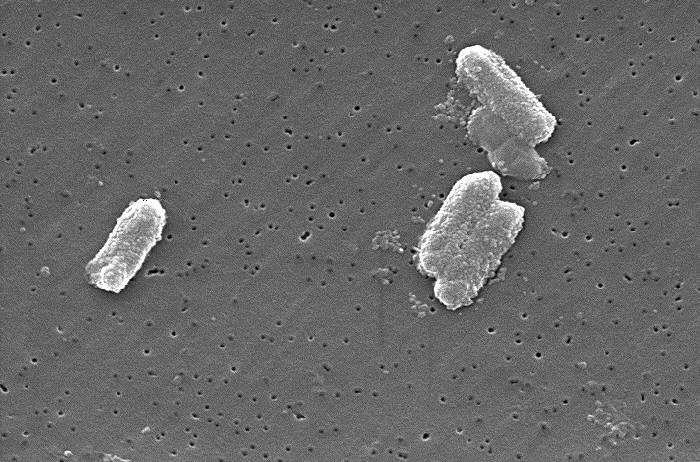
Bacterial and fungal cells are mostly water and have low contrast against the glass slide background. Without staining:
- You can’t distinguish cell shape (cocci vs. rods)
- You can’t tell if a microbe has a thick or thin cell wall
- You can’t differentiate live from dead cells
- You can’t detect hard-to-see pathogens like Mycobacterium tuberculosis
Stains bind to specific cellular components—like peptidoglycan, lipids, or DNA—making microbes visible, identifiable, and classifiable within minutes.
The Big Four: Core Staining Techniques in Clinical Microbiology
1. Gram Stain – The Gold Standard
Developed in 1884 by Danish scientist Hans Christian Gram, this is the first test performed on almost every bacterial sample in a clinical lab.
How it works:
- Cells are stained with crystal violet (purple dye)
- Iodine is added to form a dye-iodine complex
- Alcohol or acetone decolorizes cells
- Safranin (red dye) is applied as a counterstain
Results:
- Gram-positive bacteria: Retain purple dye (thick peptidoglycan layer traps the complex)
→ Staphylococcus, Streptococcus, Bacillus - Gram-negative bacteria: Lose purple, take up red (thin peptidoglycan + outer membrane)
→ E. coli, Pseudomonas, Salmonella
Clinical impact:
A Gram stain of sputum, blood, or cerebrospinal fluid can guide emergency antibiotic therapy within 15 minutes—long before culture results arrive.
💡 Pro tip: Gram stain also reveals white blood cells, helping distinguish infection from contamination.
2. Acid-Fast Stain – For Tough, Waxy Pathogens
Some bacteria, like Mycobacterium tuberculosis (TB) and M. leprae (leprosy), have waxy, lipid-rich cell walls full of mycolic acids. These resist standard stains and even many disinfectants.
Two main methods:
- Ziehl-Neelsen (hot stain): Uses heat to drive carbol fuchsin (red dye) into the cell
- Kinyoun (cold stain): Uses a higher dye concentration without heat
After staining, acid-alcohol is applied. Acid-fast bacteria retain the red dye; non-acid-fast cells lose color and take up a blue counterstain (methylene blue).
Result:
- Acid-fast bacilli (AFB): Bright red rods
- Non-acid-fast: Blue
Why it matters:
In regions with high TB burden, a quick AFB smear can trigger isolation and treatment before molecular tests confirm the diagnosis.
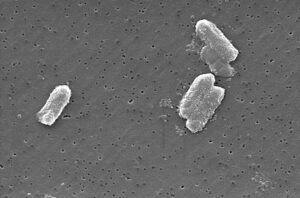
3. Simple Stains – Quick and Informative
Sometimes, you just need to see shape and arrangement—not cell wall type.
Common dyes: Methylene blue, crystal violet, safranin
Process: Apply one dye → rinse → dry → observe
Use cases:
- Checking bacterial morphology in urine or wound samples
- Teaching labs (easy for beginners)
- Rapid assessment of fungal elements (e.g., yeast vs. hyphae)
While simple, this method lacks the discriminatory power of differential stains like Gram or acid-fast.
4. Special Stains – Targeting Specific Structures
These highlight particular features that standard stains miss:
| STAIN | TARGET | USE CASE |
|---|---|---|
| India ink | Capsule (negative stain) | DetectCryptococcus neoformansin CSF (appears as a clear halo around yeast) |
| Lactophenol cotton blue | Fungal cell walls | Visualize molds in culture (stains chitin blue) |
| Giemsa stain | Parasites & blood cells | IdentifyPlasmodium(malaria),Trypanosoma, andLeishmania |
| Calcofluor white | Fungal chitin (fluorescent) | Rapid detection of fungi in tissue under UV light |
| Endospore stain (Schaeffer-Fulton) | Bacterial spores | DetectBacillusorClostridiumspores (green spores in red cells) |
🔬 Fun fact: Calcofluor white binds to chitin and cellulose—so it also stains plant fibers! Always confirm with morphology.
Advanced Staining: Fluorescence and Immunology
Modern labs increasingly use fluorescent and antibody-based stains for speed and specificity.
Fluorescent Stains
- DAPI: Binds DNA—lights up all cells under UV
- Acridine orange: Stains nucleic acids; bacteria glow orange, fungi green
- Auramine-rhodamine: Used for TB screening—faster and more sensitive than Ziehl-Neelsen
Immunofluorescence (IF)
Uses antibodies tagged with fluorescent dyes to target specific pathogens:
- Direct IF: Labeled antibody binds directly to the microbe
- Indirect IF: Uses a secondary labeled antibody for signal amplification
Applications:
- Rapid diagnosis of Legionella in sputum
- Detecting viral antigens (e.g., rabies in brain tissue)
- Identifying Pneumocystis jirovecii in immunocompromised patients
Common Pitfalls & Best Practices
Even experienced techs can make staining errors. Watch out for:
🚫 Over-decolorizing in Gram stain → Gram-positives appear falsely Gram-negative
🚫 Old cultures → Gram-positives may lose cell wall integrity and stain poorly
🚫 Contaminated reagents → False positives or background staining
🚫 Inadequate fixation → Cells wash away during staining
Best practices:
- Use fresh cultures (<24–48 hours old)
- Include control slides (known Gram+ and Gram– strains)
- Standardize decolorization time (5–15 seconds is typical)
- Train staff regularly—staining is both science and art
Why Staining Still Matters in the Age of PCR and Sequencing
You might wonder: With rapid PCR, MALDI-TOF, and whole-genome sequencing, do we still need stains?
Yes—more than ever.
Here’s why:
- Speed: Staining gives answers in minutes, not hours or days
- Cost: A Gram stain costs pennies; molecular tests cost dollars
- Context: Stains show host response (e.g., pus cells) and microbe morphology—critical for interpreting molecular results
- Resource-limited settings: Staining requires only a microscope and basic dyes—making it globally accessible
In fact, the WHO lists microscopy with staining as an essential diagnostic tool for TB, malaria, and fungal infections in low-income countries.
Final Thought: The Art of Seeing the Unseen
Staining transforms the invisible into the intelligible. It’s where chemistry meets biology, and where a single drop of dye can reveal the difference between a harmless contaminant and a life-threatening pathogen.
For students, it’s a rite of passage. For clinicians, it’s a lifeline. And for microbiologists, it’s a daily reminder that sometimes, the oldest tools are still the sharpest.
Want More Lab Insights?
At ClinicalMicrobiology.org, we break down complex lab techniques into clear, actionable knowledge for healthcare professionals and scientists.
👉 Subscribe for guides on culture methods, antimicrobial testing, emerging pathogens, and more—delivered straight to your inbox.
Note: This article is original content created for educational purposes. All staining protocols referenced follow standard clinical microbiology guidelines (e.g., CLSI, CDC, WHO).






Post Comment