mRNA Vaccines Outperform Natural Infection in Boosting Killer T Cells Against COVID-19
Why mRNA Vaccines Are Better Than Natural Infection at Training Killer T Cells
For years, scientists have debated: Is natural immunity from a past infection better than vaccine-induced protection? A landmark study from Stanford Medicine offers a clear answer—at least when it comes to killer T cells, a critical arm of the immune system.
The research, published in Immunity, reveals that the Pfizer-BioNTech mRNA vaccine does a far better job than natural SARS-CoV-2 infection at activating killer T cells—specialized immune cells that destroy virus-infected cells and help prevent long-term complications like long COVID.
Even more striking: people who had already recovered from COVID-19 showed a weaker killer T cell response after vaccination compared to those who were vaccinated before ever getting infected.
What Are Killer T Cells—and Why Do They Matter?
Most people know about antibodies—Y-shaped proteins that block viruses from entering cells. But antibodies can’t eliminate a virus once it’s already inside.
That’s where killer T cells (also called cytotoxic T cells) come in. These immune warriors patrol the body, scanning cells for signs of infection. When they spot a cell hijacked by a virus like SARS-CoV-2, they destroy it—stopping the virus from multiplying and spreading.
“Only killer T cells can clear an established infection,” says Dr. Mark Davis, senior author of the study and a leading immunologist at Stanford.
This makes them essential not just for recovery—but for preventing persistent infection, which may contribute to long COVID.
mRNA Vaccines Trigger a Powerful T Cell Response
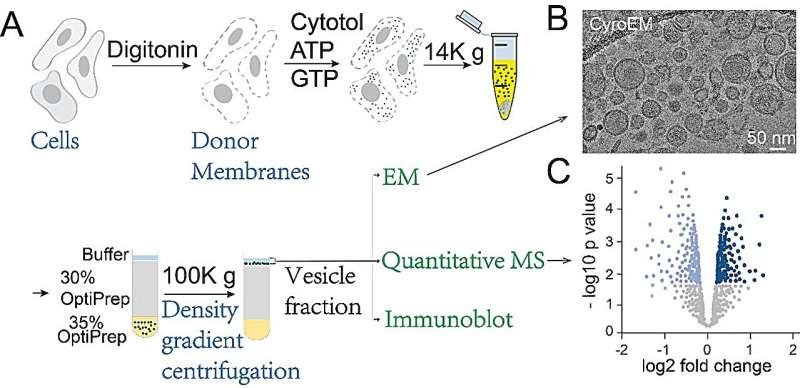
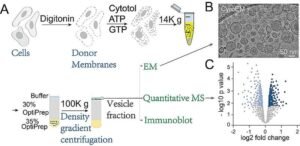
Using advanced lab techniques developed in Davis’s lab, researchers tracked SARS-CoV-2-specific killer T cells in three groups:
- Never-infected people receiving two mRNA vaccine doses
- Unvaccinated people with active COVID-19
- Recovered patients later receiving the vaccine
The results were striking:
- In never-infected vaccine recipients, killer T cells targeting SARS-CoV-2 increased more than 60-fold.
- Within six weeks, 1 in 5 of their killer T cells was trained to fight the virus.
- In contrast, people who had COVID-19—even after vaccination—had less than 1/7th as many virus-specific killer T cells.
- Their T cells also appeared less active, producing fewer immune-signaling molecules needed for a strong attack.
This happened even though natural infection exposes the immune system to many viral proteins, while the mRNA vaccine only delivers instructions for the spike protein.
Prior Infection Blunts the Vaccine’s T Cell Boost
One of the study’s most important findings: getting infected before vaccination weakens the immune system’s ability to build a robust killer T cell army.
While vaccination after infection still provides some benefit—especially for antibody production—it doesn’t fully restore killer T cell function.
Dr. Davis suggests this impaired response may help explain why some people develop long COVID:
“If killer T cells are exhausted or too few, they can’t eliminate all infected cells. The virus may linger, causing ongoing symptoms.”
Antibodies vs. T Cells: Two Layers of Defense
It’s worth noting that antibody responses remain strong even after prior infection. Helper T cells—which support antibody production—were also largely unaffected.
But antibodies alone aren’t enough. They’re great at preventing infection, but useless once the virus is inside cells.
“Antibodies block the door. Killer T cells clean house,” explains the research team.
That’s why a strong T cell response is crucial for complete immune protection—especially against evolving variants that can dodge antibodies.
Implications for Public Health and Clinical Practice
This study reinforces a key public health message: get vaccinated before exposure if possible. Vaccination primes the immune system to respond faster, stronger, and more completely.
For clinicians and microbiologists, the findings highlight the need to look beyond antibodies when evaluating immunity. T cell assays—though more complex—are essential for a full picture of immune readiness.
As Dr. Davis notes:
“T cells recognize parts of the virus that don’t change easily. That makes them more resilient against new variants than antibodies.”
Final Takeaway: Vaccination Is the Smartest Immune Strategy
Natural infection may seem like a “free” way to gain immunity—but this research shows it comes at a cost. It leaves the immune system less prepared to fight future threats.
In contrast, mRNA vaccination builds a more effective, durable, and balanced defense—especially in the critical killer T cell compartment.
For anyone hoping to avoid severe illness, reinfection, or long-term complications, vaccination remains the best first line of defense.
Stay Updated on Immune Science & Microbiology
At ClinicalMicrobiology.org, we translate cutting-edge research into clear insights for clinicians, scientists, and health professionals.
👉 Subscribe to our newsletter to get the latest on immunology, infectious disease, and vaccine science—explained simply, without the jargon.
Note: This article is based on original reporting by Stanford Medicine (March 28, 2023). All scientific credit belongs to Dr. Mark Davis and his team. Content has been fully rewritten for clarity, originality, and educational value.








Post Comment