HYPOTHETICAL OUTBREAK INVESTIGATION INTO GUINEA WORM DISEASE

HYPOTHETICAL OUTBREAK INVESTIGATION INTO GUINEA WORM DISEASE
Introduction and epidemiological features
Guinea worm disease (GWD) is both one of many neglected tropical diseases that is driven primarily by poor environmental conditions. It remains a significant threat because of the possibility of resurgence given the impending threat of climate change. While almost entering the history books as another success of disease eradication in the world, Guinea worm disease (Dracunculus medinensis) is making a potential come back. It is thought that the disease got its name from the Gulf of Guinea, including the area that is now south-eastern Nigeria1. The disease caused by Dracunculus medinensis is called dracunculiasis and is a debilitating and painful condition that is often crippling for the patient. While the disease is only rarely fatal, the crippling inability to function normally makes the morbidity very high2. The year 2017 was a significant milestone for the Guinea Worm Eradication Program (GWEP) as it had succeeded in reducing the burden of the disease from about four million cases across 21 countries to 30 cases. This celebrated success was however short lived as cases soon began to increase again.
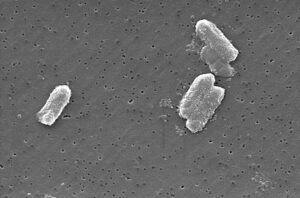
The cause is Dracunculus medinensis – a helminth is approximately 2mm wide, and 80cm long (males much shorter than females)3. New evidence shows that dogs may be reservoirs of infection; so also frogs and fish4.
The disease can occur in any age group but frequently presents in adolescents and young adults aged 15 to 45 years. Both genders are equally affected although some studies showed a slightly male predominance5.
Dracunculiasis occurs where there are ponds, pools or shallow wells contaminated with infected copepods and is most prevalent in sub-Saharan Africa6. Most infections occur in poor villages without good quality water for drinking, and people uninformed of its mode of acquisition and prevention.7 The peak of infection is during rainy season peak July to September8,9
Humans as definitive hosts acquire the infection after drinking water contaminated with infected copepods. They remain asymptomatic with the helminths in the subcutaneous tissue. About one year later, gravid females go the lower limbs to shed thousands of rhabditiform larvae through blisters which erupt on contact with fresh water. These larvae are swallowed by copepods and the larvae migrate to copepod tissue. The cycle continues when humans ingest this contaminated water. Clinical feature includes pain as helminth migrates through joints, non-specific fever, malaise, and blister with emerging worm9.
OUTBREAK INVESTIGATION STEPS
Hypothetical scenario: I have been invited to investigate a potential increase in the number of Guinea worm (GW) cases in the remote villages at the Western province of Rwanda. While only two cases were reported from July to September the preceding year, this year, in August, there are 10 reported cases. I appointed to lead the team to investigate the outbreak.
Planning the investigation
I will need materials and manpower to conduct outbreak investigation. These are listed in table below with justification for the needs.
Table 1; Requirements for conducting GWD outbreak investigation
| Staff | Justification | Materials | Justification |
| Guinea worm focal person or designate from FMOH | Knowledgeable about federal epidemiology | Transport – 4WD for the terrain, geographic mapping application, digital compass, internet location | Rocky untarred road with difficult access |
| Physician – preferably with expertise | Diagnosis and treatment | Questionnaires | Data collection |
| State/Local government DSNO | Knowledgeable about local epidemiology | Educational charts/posters | Health promotion |
| Social worker/ Nurse | Management and psycho-support support and health promotion activities | Generator for electricity if needed | Power microscope, and communication equipment like phones |
| Epidemiologist | Data collection and analysis | Kola nut to give traditional leaders | Sign of courtesy to gain acceptance and trust of community |
| Lab technician | Examine specimen and rule out differential diagnosis | Water filters | Health promotion |
| Medical microbiologist | Coordination of interlink between clinical and laboratory information | Microscope, Slides and cover slips | Microscopy |
| DSNO = Disease Surveillance and Notification Officer | |||
Initial investigation to confirm diagnosis.
Guinea worm disease in primarily diagnosed from history and clinical features. If a history is elicited of emerging worm from blisters in lower limb or any part of the body in an endemic region, the diagnosis can be made3. Other features to increase the evidence of GW itching of site followed byblister with intense urticaria preceding emergence of the worm3. Examination of the blisters or site of emergence of worm give unspecific hints and this can further be complicated when there is superimposed bacterial infection or inflammation/cellulitis at site9. Visualization of rhabditiform larvae is possible; a suspected limb with blister can be placed in a container of fresh water, as the blister erupts, the female will shed the larvae. These can be collected in a universal tube and viewed under low magnification with the microscope3,10. These can be identified by their characteristic morphology and rhabditiform shaped pharynx11. The adult female worm may be seen emerging, and the worm rolled round a matchstick very slowly over days for visualization9. Ancillary investigation includes peripheral blood film for eosinophilia9. Because the occurrence of blisters and viewing emerging worms is sporadic, verbal questioning about cases is needed. This snow balling method may lead to visits to a neighbouring hamlet. Case search is best directed at those sharing the same water source as first cases/cases found.
Confirmation of outbreak
Once there is sufficient evidence that the diagnosis is GWD, there should be verification that the numbers are above the endemic rate. This will be done by taking data from the local primary healthcare centre, verbal reports from community informants and verbal autopsy.
Notification once diagnosis is confirmed.
Once there is evidence of increased rates, communication through the formal channels upwards while we continue case investigation, line list and management of cases. Distributing filters and education will be done and we may ask for additional staff from federal state and LGA if magnitude is high.
Disease specifics for mapping
Because guinea worm occurs in clusters usually, we will define the specific locations affected and map them out. It may be possible to map to specific water ponds or lakes that is in common use. Because girls are often the ones who fetch water for households, they may be disproportionately affected. Data from clinics around vicinity over the past year and school absenteeism because of leg pain and blisters can be obtained.
Case definitions12
Confirmed case: infection occurring in a person with skin lesions with emergence of one or more worms – can be from history.
Indigenous case: A case that has not travelled outside the locality for at least one year.
Suspected case: Those with informal information that worms emerged.
Endemic village: Report of active case in the preceding year
Data collection and analysis
Expanded data collection from initial investigation is needed. The data will be collected by trained field workers from clinics, dispensaries, and schools in relative proximity to the mapped contaminated water. Data collected will include basic demographics, contact and source of water, water treatment plan, visitations to houses and houses or community water. History of travel to endemic area.
The map of area will be obtained from Central Health Authority and geographic location system used to map out clusters affected and water source-spot map. The line list will also be mapped according to water contact and overlayed on former map to detect cluster patterns associated.
Prevention interventions like use of temphos12 in contaminated pools, cloth filters and management of super-imposed bacterial infection will be done. We will continue surveillance and treatment until all affected clusters and people affected are identified.
Information Dissemination
Continuous reporting on surveillance, management and treatment and progress of the team will be made twice weekly. The Central and local departments at various levels will receive and disseminate to stakeholders such as NGOs.
FACTORS RESPONSIBLE FOR OCCURRENCE OF DRACUNCULIASIS
Factors responsible for GWD are multifactorial but in general feed into use of water with GW infected copepods. This essentially occurs because of unavailability/inaccessibility of good drinking water. The greatest risk factor for GWD is having disease the preceding year13.
- Drinking water source being ponds, drying riverbeds with infected copepods
- Eating any liquid of food’s possibly contaminated with infected copepods
- Unavailability of protected water source at boreholes or hand dug wells that are free from contamination increases risk.
- Lack of awareness creation via media/telegram flyers and town criers to educate people especially those in remote area the risk factors and prevention of spread of this disease.
- Lack of knowledge/compliance of people with swelling and wound from not entering ponds and other water used for drinking.
- Unavailability or use of torn of cloth filters
- Behavioural factors
- biological – keeping dog population14
- Travel to endemic area
- Consumption of improperly cooked un-gutted fish
- Geography: The life cycle is maintained by specific geographical conditions.
- elevation, climate, precipitation, temperature because of their relationship with water/rain availability
- water sources factors15.
- Poor governance with inability to provide basic necessities like clean drinking water
- Poor education
- Poor health habits
- Flooding
- Poor socioeconomic status
- Inability to treat water with temephos
- Occupation – water fetchers, hunters, farmers and herders who drink contaminated water when in bushes.

Figure 1:Illustration of conceptual model of GWD control
A multipronged approach may be needed to curb GWD. The most widely used strategy has been primarily preventing copepod contact with humans (cloth filters) combined with copepod elimination from water (chemical treatment) with some degree of success. A wider model is needed to eliminate the disease. The following approaches should all be considered together.
The Agent
- Chemical control with temephos performed monthly. It is a kills copepod without being harmful to humans and animals. The monthly protocol starts a month before transmission season and ends a month after. This method is used when the water source is 500m3 or less. It is used while better and safer water sources like borehole are awaited. Temephos is said to have cost-benefit ratio of 4.14 when contrasted with other control measures16. It is associate with discolouration of water for 4-8 hours. Chlorination is an alternative chemical but with more undesirable effects.
- Boiling is also effective use of firewood is disadvantageous to environment3,7.
- Nylon cloth use is very effective and was one of the key strategies used with successful reduction of cases17.
The host
- Adult parasite removal as described previously will prevent shedding into drinking water of GW larvae. Extraction takes 1-2 months as GW is rolled by few cm daily, wound wrapped with bandage and patient asked not to move around much especially not to enter water sources.
- Surveillance and reporting are key to identification of cases without which spread would have occurred. Communities should encourage and reward/ give incentives for voluntary reporting of GWD cases, every case should aim to be targeted within 24 hours.
- Case containment will prevent by regular cleansing and covering affected limb until worm is completely removed.
- Regular use of water from safe water sources should be encouraged even if it requires going the extra mile.
- Where conventional safe water sources are not available, safe water that has been filtered, boiled, chlorinated or has had temephos added is key not acquiring infection Education as some believe it is passed down through generations5,6.
- Safe food preparation by avoiding uncooked/un-gutted fish may decrease disease acquisition18
The Environment
- Water source protection by barricading surrounding of hand dug wells/ ponds to prevent entry of infected persons17.
- Provision of boreholes.
Investigations of causes of increase in GWD in the locality
The most common problems to be investigated include:
- Borewell/borehole problems:
- Total lack of
- Spoilt
- Located faraway.
- Fee for water fetching.
- Drought decreasing water level.
- Flooding during rainy season allowing for mixture of water sources. May result from climate change17.
- Case reporting problems
- No community case reporting
- Lack of village reporting officers19.
- Water filtration problems
- Lack of cloth filters
- Torn cloth filters
- Lack of knowledge of cloth filter importance
- Security problems like kidnapping/ banditry preventing people from walking to collect water.
- Immigration from endemic to non-endemic village or travel to those villages and returning with infection.
- Change in behaviour – those below still being investigated20.
- Eating improperly cooked un-gutted fish or frogs.
- Increased dog, ferret or monkey keeping if they are fed fish entrails.
Three potential reasons for the increase in cases
There may have been recent immigration of people from other endemic areas, change in behaviour such as increased dog keeping or eating improperly cooked un-gutted fish. These add to the storm in a setting of an already poor control program. Specific control program deficiencies include that could make most impact include:
- Lack of chemical treatment of water: In the multipronged approach, the use of temephos is one very vital element. This especially because is fast, relatively easy, effective, and cost-effective. It is certainly the emergency stop gap.
- Lack of adequate surveillance/reporting of any case detected combined with these cases entering fresh water sources and enabling continuation of the life cycle of GW. Also contributing here is poor education about GWD prevention because of defective or non-existent health promotion activities as the community could potentially be their brother’s keeper by preventing affected individuals from shedding larvae in water sources.
- Lack of safe drinking water because of; lack of protected borewells/boreholes, inability to boil water, unavailability of good nylon filtration cloths.
The three top recommendations to the Ministry of Health should be
- Increasing access to safe drinking water in a cost effective and equitable manner in collaboration with Ministry of Water.
- Decrease copepod infestation of water by using temephos. This can be staggered with the aim of achieving full and optimal temephos use monthly beginning a month and continuing monthly until a month after rainy season.
- Ensure detection of cases within 24-hours and notify health authorities for immediate case control. This is best by dedicating disease surveillance notification officers to endemic villages and having case management team reach village and commence management 24-hours after receiving information.
Other important aspects to considered as low hanging fruit include.
- Protect water sources with barriers, use of filter cloths, and health education.
The goals the Ministry will be advised to set include –
- To collaborate with Ministry of Water to ensure construction of at least one hand pump borewell in each endemic village within the next one year (May 2022) and scale up in two years (May 2023) to increase borewell in endemic villages to one borewell per 100 population.
- Administer correctly at least two rounds of correctly applied temephos in each endemic village during the next rainy season (April – September 2021) and scale up to administering four rounds in rainy season of 2022 and subsequently administering complete eight rounds during rainy season o 2023.
- Employ at least one community disease surveillance and notification officer in each endemic village whose role is to ensure all cases are reported within 24 hours. This employment and training should be completed, and officers deployed before beginning of rainy season by March 2022.
REFERENCES
1. Greenwood, B., Greenwood, A. & Bradley, A. Guinea worm infection in northern Nigeria: reflections on a disease approaching eradication. Trop. Med. Int. Heal. 22, 558–566 (2017).
2. Dracunculiasis (guinea-worm disease). https://www.who.int/news-room/fact-sheets/detail/dracunculiasis-(guinea-worm-disease).
3. Cairncross, S., Muller, R. & Zagaria, N. Dracunculiasis (guinea worm disease) and the eradication initiative. Clinical Microbiology Reviews vol. 15 223–246 (2002).
4. Cleveland, C. A. et al. A search for tiny dragons (Dracunculus medinensis third-stage larvae) in aquatic animals in Chad, Africa. Sci. Rep. 9, 1–7 (2019).
5. Nwoke, B. E. Behavioural aspects and their possible uses in the control of dracontiasis (guinea-worm) in Igwun river basin area of Imo State, Nigeria. Angew. Parasitol. 33, 205–210 (1992).
6. Microbial fact sheets – Guidelines for Drinking-Water Quality: Fourth Edition Incorporating the First Addendum – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK442360/.
7. Ruiz-Tiben, E. & Hopkins, D. R. Dracunculiasis (Guinea Worm Disease) Eradication. Advances in Parasitology (2006) doi:10.1016/S0065-308X(05)61007-X.
8. (No Title). https://www.cartercenter.org/resources/pdfs/news/features/guinea_worm/gw-maps-1986-2010.pdf.
9. Parenti, D. M. Dracunculiasis. in Medical Parasitology 58–62 (CRC Press, 2009). doi:10.1201/9781498713672-18.
10. Muller, R. Guinea worm disease: Epidemiology, control and treatment. Bull. World Health Organ. 57, 683–689 (1979).
11. Dracunculus. https://parasite.org.au/para-site/text/dracunculus-text.html.
12. Hopkins, D. R., Ruiz-Tiben, E., Eberhard, M. L., Roy, S. L. & Weiss, A. J. Progress Toward Global Eradication of Dracunculiasis, January 2016–June 2017. MMWR. Morb. Mortal. Wkly. Rep. 66, 1327–1331 (2017).
13. Prevention, C.-C. for D. C. and. CDC – Guinea Worm Disease – Epidemiology & Risk Factors. (2019).
14. Guagliardo, S. A. J. et al. Guinea worm in domestic dogs in chad: A description and analysis of surveillance data. PLoS Negl. Trop. Dis. 14, 1–17 (2020).
15. Richards, R. L. et al. Identifying correlates of Guinea worm (Dracunculus medinensis) infection in domestic dog populations. PLoS Negl. Trop. Dis. 14, e0008620 (2020).
16. WHO | Chemical control of copepods. WHO (2017).
17. Netshikweta, R. & Garira, W. A Multiscale Model for the World’s First Parasitic Disease Targeted for Eradication: Guinea Worm Disease. Comput. Math. Methods Med. 2017, (2017).
18. Prevention, C.-C. for D. C. and. CDC – Guinea Worm Disease – General Information – Frequently Asked Questions (FAQs). (2020).
19. Cairncross, S., Braide, E. I. & Bugri, S. Z. Community participation in the eradication of guinea worm disease. Acta Trop. 61, 121–136 (1996).
20. Eberhard, M. L. et al. Possible role of fish and frogs as paratenic hosts of Dracunculus medinensis, Chad. Emerg. Infect. Dis. 22, 1428–1430 (2016).

HYPOTHETICAL OUTBREAK INVESTIGATION INTO GUINEA WORM DISEASE
Introduction and epidemiological features
Guinea worm disease (GWD) is both one of many neglected tropical diseases that is driven primarily by poor environmental conditions. It remains a significant threat because of the possibility of resurgence given the impending threat of climate change. While almost entering the history books as another success of disease eradication in the world, Guinea worm disease (Dracunculus medinensis) is making a potential come back. It is thought that the disease got its name from the Gulf of Guinea, including the area that is now south-eastern Nigeria1. The disease caused by Dracunculus medinensis is called dracunculiasis and is a debilitating and painful condition that is often crippling for the patient. While the disease is only rarely fatal, the crippling inability to function normally makes the morbidity very high2. The year 2017 was a significant milestone for the Guinea Worm Eradication Program (GWEP) as it had succeeded in reducing the burden of the disease from about four million cases across 21 countries to 30 cases. This celebrated success was however short lived as cases soon began to increase again.
The cause is Dracunculus medinensis – a helminth is approximately 2mm wide, and 80cm long (males much shorter than females)3. New evidence shows that dogs may be reservoirs of infection; so also frogs and fish4.
The disease can occur in any age group but frequently presents in adolescents and young adults aged 15 to 45 years. Both genders are equally affected although some studies showed a slightly male predominance5.
Dracunculiasis occurs where there are ponds, pools or shallow wells contaminated with infected copepods and is most prevalent in sub-Saharan Africa6. Most infections occur in poor villages without good quality water for drinking, and people uninformed of its mode of acquisition and prevention.7 The peak of infection is during rainy season peak July to September8,9
Humans as definitive hosts acquire the infection after drinking water contaminated with infected copepods. They remain asymptomatic with the helminths in the subcutaneous tissue. About one year later, gravid females go the lower limbs to shed thousands of rhabditiform larvae through blisters which erupt on contact with fresh water. These larvae are swallowed by copepods and the larvae migrate to copepod tissue. The cycle continues when humans ingest this contaminated water. Clinical feature includes pain as helminth migrates through joints, non-specific fever, malaise, and blister with emerging worm9.
OUTBREAK INVESTIGATION STEPS
Hypothetical scenario: I have been invited to investigate a potential increase in the number of Guinea worm (GW) cases in the remote villages at the Western province of Rwanda. While only two cases were reported from July to September the preceding year, this year, in August, there are 10 reported cases. I appointed to lead the team to investigate the outbreak.
Planning the investigation
I will need materials and manpower to conduct outbreak investigation. These are listed in table below with justification for the needs.
Table 1; Requirements for conducting GWD outbreak investigation
| Staff | Justification | Materials | Justification |
| Guinea worm focal person or designate from FMOH | Knowledgeable about federal epidemiology | Transport – 4WD for the terrain, geographic mapping application, digital compass, internet location | Rocky untarred road with difficult access |
| Physician – preferably with expertise | Diagnosis and treatment | Questionnaires | Data collection |
| State/Local government DSNO | Knowledgeable about local epidemiology | Educational charts/posters | Health promotion |
| Social worker/ Nurse | Management and psycho-support support and health promotion activities | Generator for electricity if needed | Power microscope, and communication equipment like phones |
| Epidemiologist | Data collection and analysis | Kola nut to give traditional leaders | Sign of courtesy to gain acceptance and trust of community |
| Lab technician | Examine specimen and rule out differential diagnosis | Water filters | Health promotion |
| Medical microbiologist | Coordination of interlink between clinical and laboratory information | Microscope, Slides and cover slips | Microscopy |
| DSNO = Disease Surveillance and Notification Officer | |||
Initial investigation to confirm diagnosis.
Guinea worm disease in primarily diagnosed from history and clinical features. If a history is elicited of emerging worm from blisters in lower limb or any part of the body in an endemic region, the diagnosis can be made3. Other features to increase the evidence of GW itching of site followed byblister with intense urticaria preceding emergence of the worm3. Examination of the blisters or site of emergence of worm give unspecific hints and this can further be complicated when there is superimposed bacterial infection or inflammation/cellulitis at site9. Visualization of rhabditiform larvae is possible; a suspected limb with blister can be placed in a container of fresh water, as the blister erupts, the female will shed the larvae. These can be collected in a universal tube and viewed under low magnification with the microscope3,10. These can be identified by their characteristic morphology and rhabditiform shaped pharynx11. The adult female worm may be seen emerging, and the worm rolled round a matchstick very slowly over days for visualization9. Ancillary investigation includes peripheral blood film for eosinophilia9. Because the occurrence of blisters and viewing emerging worms is sporadic, verbal questioning about cases is needed. This snow balling method may lead to visits to a neighbouring hamlet. Case search is best directed at those sharing the same water source as first cases/cases found.
Confirmation of outbreak
Once there is sufficient evidence that the diagnosis is GWD, there should be verification that the numbers are above the endemic rate. This will be done by taking data from the local primary healthcare centre, verbal reports from community informants and verbal autopsy.
Notification once diagnosis is confirmed.
Once there is evidence of increased rates, communication through the formal channels upwards while we continue case investigation, line list and management of cases. Distributing filters and education will be done and we may ask for additional staff from federal state and LGA if magnitude is high.
Disease specifics for mapping
Because guinea worm occurs in clusters usually, we will define the specific locations affected and map them out. It may be possible to map to specific water ponds or lakes that is in common use. Because girls are often the ones who fetch water for households, they may be disproportionately affected. Data from clinics around vicinity over the past year and school absenteeism because of leg pain and blisters can be obtained.
Case definitions12
Confirmed case: infection occurring in a person with skin lesions with emergence of one or more worms – can be from history.
Indigenous case: A case that has not travelled outside the locality for at least one year.
Suspected case: Those with informal information that worms emerged.
Endemic village: Report of active case in the preceding year
Data collection and analysis
Expanded data collection from initial investigation is needed. The data will be collected by trained field workers from clinics, dispensaries, and schools in relative proximity to the mapped contaminated water. Data collected will include basic demographics, contact and source of water, water treatment plan, visitations to houses and houses or community water. History of travel to endemic area.
The map of area will be obtained from Central Health Authority and geographic location system used to map out clusters affected and water source-spot map. The line list will also be mapped according to water contact and overlayed on former map to detect cluster patterns associated.
Prevention interventions like use of temphos12 in contaminated pools, cloth filters and management of super-imposed bacterial infection will be done. We will continue surveillance and treatment until all affected clusters and people affected are identified.
Information Dissemination
Continuous reporting on surveillance, management and treatment and progress of the team will be made twice weekly. The Central and local departments at various levels will receive and disseminate to stakeholders such as NGOs.
FACTORS RESPONSIBLE FOR OCCURRENCE OF DRACUNCULIASIS
Factors responsible for GWD are multifactorial but in general feed into use of water with GW infected copepods. This essentially occurs because of unavailability/inaccessibility of good drinking water. The greatest risk factor for GWD is having disease the preceding year13.
- Drinking water source being ponds, drying riverbeds with infected copepods
- Eating any liquid of food’s possibly contaminated with infected copepods
- Unavailability of protected water source at boreholes or hand dug wells that are free from contamination increases risk.
- Lack of awareness creation via media/telegram flyers and town criers to educate people especially those in remote area the risk factors and prevention of spread of this disease.
- Lack of knowledge/compliance of people with swelling and wound from not entering ponds and other water used for drinking.
- Unavailability or use of torn of cloth filters
- Behavioural factors
- biological – keeping dog population14
- Travel to endemic area
- Consumption of improperly cooked un-gutted fish
- Geography: The life cycle is maintained by specific geographical conditions.
- elevation, climate, precipitation, temperature because of their relationship with water/rain availability
- water sources factors15.
- Poor governance with inability to provide basic necessities like clean drinking water
- Poor education
- Poor health habits
- Flooding
- Poor socioeconomic status
- Inability to treat water with temephos
- Occupation – water fetchers, hunters, farmers and herders who drink contaminated water when in bushes.

Figure 1:Illustration of conceptual model of GWD control
A multipronged approach may be needed to curb GWD. The most widely used strategy has been primarily preventing copepod contact with humans (cloth filters) combined with copepod elimination from water (chemical treatment) with some degree of success. A wider model is needed to eliminate the disease. The following approaches should all be considered together.
The Agent
- Chemical control with temephos performed monthly. It is a kills copepod without being harmful to humans and animals. The monthly protocol starts a month before transmission season and ends a month after. This method is used when the water source is 500m3 or less. It is used while better and safer water sources like borehole are awaited. Temephos is said to have cost-benefit ratio of 4.14 when contrasted with other control measures16. It is associate with discolouration of water for 4-8 hours. Chlorination is an alternative chemical but with more undesirable effects.
- Boiling is also effective use of firewood is disadvantageous to environment3,7.
- Nylon cloth use is very effective and was one of the key strategies used with successful reduction of cases17.
The host
- Adult parasite removal as described previously will prevent shedding into drinking water of GW larvae. Extraction takes 1-2 months as GW is rolled by few cm daily, wound wrapped with bandage and patient asked not to move around much especially not to enter water sources.
- Surveillance and reporting are key to identification of cases without which spread would have occurred. Communities should encourage and reward/ give incentives for voluntary reporting of GWD cases, every case should aim to be targeted within 24 hours.
- Case containment will prevent by regular cleansing and covering affected limb until worm is completely removed.
- Regular use of water from safe water sources should be encouraged even if it requires going the extra mile.
- Where conventional safe water sources are not available, safe water that has been filtered, boiled, chlorinated or has had temephos added is key not acquiring infection Education as some believe it is passed down through generations5,6.
- Safe food preparation by avoiding uncooked/un-gutted fish may decrease disease acquisition18
The Environment
- Water source protection by barricading surrounding of hand dug wells/ ponds to prevent entry of infected persons17.
- Provision of boreholes.
Investigations of causes of increase in GWD in the locality
The most common problems to be investigated include:
- Borewell/borehole problems:
- Total lack of
- Spoilt
- Located faraway.
- Fee for water fetching.
- Drought decreasing water level.
- Flooding during rainy season allowing for mixture of water sources. May result from climate change17.
- Case reporting problems
- No community case reporting
- Lack of village reporting officers19.
- Water filtration problems
- Lack of cloth filters
- Torn cloth filters
- Lack of knowledge of cloth filter importance
- Security problems like kidnapping/ banditry preventing people from walking to collect water.
- Immigration from endemic to non-endemic village or travel to those villages and returning with infection.
- Change in behaviour – those below still being investigated20.
- Eating improperly cooked un-gutted fish or frogs.
- Increased dog, ferret or monkey keeping if they are fed fish entrails.
Three potential reasons for the increase in cases
There may have been recent immigration of people from other endemic areas, change in behaviour such as increased dog keeping or eating improperly cooked un-gutted fish. These add to the storm in a setting of an already poor control program. Specific control program deficiencies include that could make most impact include:
- Lack of chemical treatment of water: In the multipronged approach, the use of temephos is one very vital element. This especially because is fast, relatively easy, effective, and cost-effective. It is certainly the emergency stop gap.
- Lack of adequate surveillance/reporting of any case detected combined with these cases entering fresh water sources and enabling continuation of the life cycle of GW. Also contributing here is poor education about GWD prevention because of defective or non-existent health promotion activities as the community could potentially be their brother’s keeper by preventing affected individuals from shedding larvae in water sources.
- Lack of safe drinking water because of; lack of protected borewells/boreholes, inability to boil water, unavailability of good nylon filtration cloths.
The three top recommendations to the Ministry of Health should be
- Increasing access to safe drinking water in a cost effective and equitable manner in collaboration with Ministry of Water.
- Decrease copepod infestation of water by using temephos. This can be staggered with the aim of achieving full and optimal temephos use monthly beginning a month and continuing monthly until a month after rainy season.
- Ensure detection of cases within 24-hours and notify health authorities for immediate case control. This is best by dedicating disease surveillance notification officers to endemic villages and having case management team reach village and commence management 24-hours after receiving information.
Other important aspects to considered as low hanging fruit include.
- Protect water sources with barriers, use of filter cloths, and health education.
The goals the Ministry will be advised to set include –
- To collaborate with Ministry of Water to ensure construction of at least one hand pump borewell in each endemic village within the next one year (May 2022) and scale up in two years (May 2023) to increase borewell in endemic villages to one borewell per 100 population.
- Administer correctly at least two rounds of correctly applied temephos in each endemic village during the next rainy season (April – September 2021) and scale up to administering four rounds in rainy season of 2022 and subsequently administering complete eight rounds during rainy season o 2023.
- Employ at least one community disease surveillance and notification officer in each endemic village whose role is to ensure all cases are reported within 24 hours. This employment and training should be completed, and officers deployed before beginning of rainy season by March 2022.
REFERENCES
1. Greenwood, B., Greenwood, A. & Bradley, A. Guinea worm infection in northern Nigeria: reflections on a disease approaching eradication. Trop. Med. Int. Heal. 22, 558–566 (2017).
2. Dracunculiasis (guinea-worm disease). https://www.who.int/news-room/fact-sheets/detail/dracunculiasis-(guinea-worm-disease).
3. Cairncross, S., Muller, R. & Zagaria, N. Dracunculiasis (guinea worm disease) and the eradication initiative. Clinical Microbiology Reviews vol. 15 223–246 (2002).
4. Cleveland, C. A. et al. A search for tiny dragons (Dracunculus medinensis third-stage larvae) in aquatic animals in Chad, Africa. Sci. Rep. 9, 1–7 (2019).
5. Nwoke, B. E. Behavioural aspects and their possible uses in the control of dracontiasis (guinea-worm) in Igwun river basin area of Imo State, Nigeria. Angew. Parasitol. 33, 205–210 (1992).
6. Microbial fact sheets – Guidelines for Drinking-Water Quality: Fourth Edition Incorporating the First Addendum – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK442360/.
7. Ruiz-Tiben, E. & Hopkins, D. R. Dracunculiasis (Guinea Worm Disease) Eradication. Advances in Parasitology (2006) doi:10.1016/S0065-308X(05)61007-X.
8. (No Title). https://www.cartercenter.org/resources/pdfs/news/features/guinea_worm/gw-maps-1986-2010.pdf.
9. Parenti, D. M. Dracunculiasis. in Medical Parasitology 58–62 (CRC Press, 2009). doi:10.1201/9781498713672-18.
10. Muller, R. Guinea worm disease: Epidemiology, control and treatment. Bull. World Health Organ. 57, 683–689 (1979).
11. Dracunculus. https://parasite.org.au/para-site/text/dracunculus-text.html.
12. Hopkins, D. R., Ruiz-Tiben, E., Eberhard, M. L., Roy, S. L. & Weiss, A. J. Progress Toward Global Eradication of Dracunculiasis, January 2016–June 2017. MMWR. Morb. Mortal. Wkly. Rep. 66, 1327–1331 (2017).
13. Prevention, C.-C. for D. C. and. CDC – Guinea Worm Disease – Epidemiology & Risk Factors. (2019).
14. Guagliardo, S. A. J. et al. Guinea worm in domestic dogs in chad: A description and analysis of surveillance data. PLoS Negl. Trop. Dis. 14, 1–17 (2020).
15. Richards, R. L. et al. Identifying correlates of Guinea worm (Dracunculus medinensis) infection in domestic dog populations. PLoS Negl. Trop. Dis. 14, e0008620 (2020).
16. WHO | Chemical control of copepods. WHO (2017).
17. Netshikweta, R. & Garira, W. A Multiscale Model for the World’s First Parasitic Disease Targeted for Eradication: Guinea Worm Disease. Comput. Math. Methods Med. 2017, (2017).
18. Prevention, C.-C. for D. C. and. CDC – Guinea Worm Disease – General Information – Frequently Asked Questions (FAQs). (2020).
19. Cairncross, S., Braide, E. I. & Bugri, S. Z. Community participation in the eradication of guinea worm disease. Acta Trop. 61, 121–136 (1996).
20. Eberhard, M. L. et al. Possible role of fish and frogs as paratenic hosts of Dracunculus medinensis, Chad. Emerg. Infect. Dis. 22, 1428–1430 (2016).

HYPOTHETICAL OUTBREAK INVESTIGATION INTO GUINEA WORM DISEASE
Introduction and epidemiological features
Guinea worm disease (GWD) is both one of many neglected tropical diseases that is driven primarily by poor environmental conditions. It remains a significant threat because of the possibility of resurgence given the impending threat of climate change. While almost entering the history books as another success of disease eradication in the world, Guinea worm disease (Dracunculus medinensis) is making a potential come back. It is thought that the disease got its name from the Gulf of Guinea, including the area that is now south-eastern Nigeria1. The disease caused by Dracunculus medinensis is called dracunculiasis and is a debilitating and painful condition that is often crippling for the patient. While the disease is only rarely fatal, the crippling inability to function normally makes the morbidity very high2. The year 2017 was a significant milestone for the Guinea Worm Eradication Program (GWEP) as it had succeeded in reducing the burden of the disease from about four million cases across 21 countries to 30 cases. This celebrated success was however short lived as cases soon began to increase again.
The cause is Dracunculus medinensis – a helminth is approximately 2mm wide, and 80cm long (males much shorter than females)3. New evidence shows that dogs may be reservoirs of infection; so also frogs and fish4.
The disease can occur in any age group but frequently presents in adolescents and young adults aged 15 to 45 years. Both genders are equally affected although some studies showed a slightly male predominance5.
Dracunculiasis occurs where there are ponds, pools or shallow wells contaminated with infected copepods and is most prevalent in sub-Saharan Africa6. Most infections occur in poor villages without good quality water for drinking, and people uninformed of its mode of acquisition and prevention.7 The peak of infection is during rainy season peak July to September8,9
Humans as definitive hosts acquire the infection after drinking water contaminated with infected copepods. They remain asymptomatic with the helminths in the subcutaneous tissue. About one year later, gravid females go the lower limbs to shed thousands of rhabditiform larvae through blisters which erupt on contact with fresh water. These larvae are swallowed by copepods and the larvae migrate to copepod tissue. The cycle continues when humans ingest this contaminated water. Clinical feature includes pain as helminth migrates through joints, non-specific fever, malaise, and blister with emerging worm9.
OUTBREAK INVESTIGATION STEPS
Hypothetical scenario: I have been invited to investigate a potential increase in the number of Guinea worm (GW) cases in the remote villages at the Western province of Rwanda. While only two cases were reported from July to September the preceding year, this year, in August, there are 10 reported cases. I appointed to lead the team to investigate the outbreak.
Planning the investigation
I will need materials and manpower to conduct outbreak investigation. These are listed in table below with justification for the needs.
Table 1; Requirements for conducting GWD outbreak investigation
|
Staff |
Justification |
Materials |
Justification |
|
Guinea worm focal person or designate from FMOH |
Knowledgeable about federal epidemiology |
Transport – 4WD for the terrain, geographic mapping application, digital compass, internet location |
Rocky untarred road with difficult access |
|
Physician – preferably with expertise |
Diagnosis and treatment |
Questionnaires |
Data collection |
|
State/Local government DSNO |
Knowledgeable about local epidemiology |
Educational charts/posters |
Health promotion |
|
Social worker/ Nurse |
Management and psycho-support support and health promotion activities |
Generator for electricity if needed |
Power microscope, and communication equipment like phones |
|
Epidemiologist |
Data collection and analysis |
Kola nut to give traditional leaders |
Sign of courtesy to gain acceptance and trust of community |
|
Lab technician |
Examine specimen and rule out differential diagnosis |
Water filters |
Health promotion |
|
Medical microbiologist |
Coordination of interlink between clinical and laboratory information |
Microscope, Slides and cover slips |
Microscopy |
|
DSNO = Disease Surveillance and Notification Officer |
|||
Initial investigation to confirm diagnosis.
Guinea worm disease in primarily diagnosed from history and clinical features. If a history is elicited of emerging worm from blisters in lower limb or any part of the body in an endemic region, the diagnosis can be made3. Other features to increase the evidence of GW itching of site followed byblister with intense urticaria preceding emergence of the worm3. Examination of the blisters or site of emergence of worm give unspecific hints and this can further be complicated when there is superimposed bacterial infection or inflammation/cellulitis at site9. Visualization of rhabditiform larvae is possible; a suspected limb with blister can be placed in a container of fresh water, as the blister erupts, the female will shed the larvae. These can be collected in a universal tube and viewed under low magnification with the microscope3,10. These can be identified by their characteristic morphology and rhabditiform shaped pharynx11. The adult female worm may be seen emerging, and the worm rolled round a matchstick very slowly over days for visualization9. Ancillary investigation includes peripheral blood film for eosinophilia9. Because the occurrence of blisters and viewing emerging worms is sporadic, verbal questioning about cases is needed. This snow balling method may lead to visits to a neighbouring hamlet. Case search is best directed at those sharing the same water source as first cases/cases found.
Confirmation of outbreak
Once there is sufficient evidence that the diagnosis is GWD, there should be verification that the numbers are above the endemic rate. This will be done by taking data from the local primary healthcare centre, verbal reports from community informants and verbal autopsy.
Notification once diagnosis is confirmed.
Once there is evidence of increased rates, communication through the formal channels upwards while we continue case investigation, line list and management of cases. Distributing filters and education will be done and we may ask for additional staff from federal state and LGA if magnitude is high.
Disease specifics for mapping
Because guinea worm occurs in clusters usually, we will define the specific locations affected and map them out. It may be possible to map to specific water ponds or lakes that is in common use. Because girls are often the ones who fetch water for households, they may be disproportionately affected. Data from clinics around vicinity over the past year and school absenteeism because of leg pain and blisters can be obtained.
Case definitions12
Confirmed case: infection occurring in a person with skin lesions with emergence of one or more worms – can be from history.
Indigenous case: A case that has not travelled outside the locality for at least one year.
Suspected case: Those with informal information that worms emerged.
Endemic village: Report of active case in the preceding year
Data collection and analysis
Expanded data collection from initial investigation is needed. The data will be collected by trained field workers from clinics, dispensaries, and schools in relative proximity to the mapped contaminated water. Data collected will include basic demographics, contact and source of water, water treatment plan, visitations to houses and houses or community water. History of travel to endemic area.
The map of area will be obtained from Central Health Authority and geographic location system used to map out clusters affected and water source-spot map. The line list will also be mapped according to water contact and overlayed on former map to detect cluster patterns associated.
Prevention interventions like use of temphos12 in contaminated pools, cloth filters and management of super-imposed bacterial infection will be done. We will continue surveillance and treatment until all affected clusters and people affected are identified.
Information Dissemination
Continuous reporting on surveillance, management and treatment and progress of the team will be made twice weekly. The Central and local departments at various levels will receive and disseminate to stakeholders such as NGOs.
FACTORS RESPONSIBLE FOR OCCURRENCE OF DRACUNCULIASIS
Factors responsible for GWD are multifactorial but in general feed into use of water with GW infected copepods. This essentially occurs because of unavailability/inaccessibility of good drinking water. The greatest risk factor for GWD is having disease the preceding year13.
- Drinking water source being ponds, drying riverbeds with infected copepods
- Eating any liquid of food’s possibly contaminated with infected copepods
- Unavailability of protected water source at boreholes or hand dug wells that are free from contamination increases risk.
- Lack of awareness creation via media/telegram flyers and town criers to educate people especially those in remote area the risk factors and prevention of spread of this disease.
- Lack of knowledge/compliance of people with swelling and wound from not entering ponds and other water used for drinking.
- Unavailability or use of torn of cloth filters
- Behavioural factors
- biological – keeping dog population14
- Travel to endemic area
- Consumption of improperly cooked un-gutted fish
- Geography: The life cycle is maintained by specific geographical conditions.
- elevation, climate, precipitation, temperature because of their relationship with water/rain availability
- water sources factors15.
- Poor governance with inability to provide basic necessities like clean drinking water
- Poor education
- Poor health habits
- Flooding
- Poor socioeconomic status
- Inability to treat water with temephos
- Occupation – water fetchers, hunters, farmers and herders who drink contaminated water when in bushes.

Figure 1:Illustration of conceptual model of GWD control
A multipronged approach may be needed to curb GWD. The most widely used strategy has been primarily preventing copepod contact with humans (cloth filters) combined with copepod elimination from water (chemical treatment) with some degree of success. A wider model is needed to eliminate the disease. The following approaches should all be considered together.
The Agent
- Chemical control with temephos performed monthly. It is a kills copepod without being harmful to humans and animals. The monthly protocol starts a month before transmission season and ends a month after. This method is used when the water source is 500m3 or less. It is used while better and safer water sources like borehole are awaited. Temephos is said to have cost-benefit ratio of 4.14 when contrasted with other control measures16. It is associate with discolouration of water for 4-8 hours. Chlorination is an alternative chemical but with more undesirable effects.
- Boiling is also effective use of firewood is disadvantageous to environment3,7.
- Nylon cloth use is very effective and was one of the key strategies used with successful reduction of cases17.
The host
- Adult parasite removal as described previously will prevent shedding into drinking water of GW larvae. Extraction takes 1-2 months as GW is rolled by few cm daily, wound wrapped with bandage and patient asked not to move around much especially not to enter water sources.
- Surveillance and reporting are key to identification of cases without which spread would have occurred. Communities should encourage and reward/ give incentives for voluntary reporting of GWD cases, every case should aim to be targeted within 24 hours.
- Case containment will prevent by regular cleansing and covering affected limb until worm is completely removed.
- Regular use of water from safe water sources should be encouraged even if it requires going the extra mile.
- Where conventional safe water sources are not available, safe water that has been filtered, boiled, chlorinated or has had temephos added is key not acquiring infection Education as some believe it is passed down through generations5,6.
- Safe food preparation by avoiding uncooked/un-gutted fish may decrease disease acquisition18
The Environment
- Water source protection by barricading surrounding of hand dug wells/ ponds to prevent entry of infected persons17.
- Provision of boreholes.
Investigations of causes of increase in GWD in the locality
The most common problems to be investigated include:
- Borewell/borehole problems:
- Total lack of
- Spoilt
- Located faraway.
- Fee for water fetching.
- Drought decreasing water level.
- Flooding during rainy season allowing for mixture of water sources. May result from climate change17.
- Case reporting problems
- No community case reporting
- Lack of village reporting officers19.
- Water filtration problems
- Lack of cloth filters
- Torn cloth filters
- Lack of knowledge of cloth filter importance
- Security problems like kidnapping/ banditry preventing people from walking to collect water.
- Immigration from endemic to non-endemic village or travel to those villages and returning with infection.
- Change in behaviour – those below still being investigated20.
- Eating improperly cooked un-gutted fish or frogs.
- Increased dog, ferret or monkey keeping if they are fed fish entrails.
Three potential reasons for the increase in cases
There may have been recent immigration of people from other endemic areas, change in behaviour such as increased dog keeping or eating improperly cooked un-gutted fish. These add to the storm in a setting of an already poor control program. Specific control program deficiencies include that could make most impact include:
- Lack of chemical treatment of water: In the multipronged approach, the use of temephos is one very vital element. This especially because is fast, relatively easy, effective, and cost-effective. It is certainly the emergency stop gap.
- Lack of adequate surveillance/reporting of any case detected combined with these cases entering fresh water sources and enabling continuation of the life cycle of GW. Also contributing here is poor education about GWD prevention because of defective or non-existent health promotion activities as the community could potentially be their brother’s keeper by preventing affected individuals from shedding larvae in water sources.
- Lack of safe drinking water because of; lack of protected borewells/boreholes, inability to boil water, unavailability of good nylon filtration cloths.
The three top recommendations to the Ministry of Health should be
- Increasing access to safe drinking water in a cost effective and equitable manner in collaboration with Ministry of Water.
- Decrease copepod infestation of water by using temephos. This can be staggered with the aim of achieving full and optimal temephos use monthly beginning a month and continuing monthly until a month after rainy season.
- Ensure detection of cases within 24-hours and notify health authorities for immediate case control. This is best by dedicating disease surveillance notification officers to endemic villages and having case management team reach village and commence management 24-hours after receiving information.
Other important aspects to considered as low hanging fruit include.
- Protect water sources with barriers, use of filter cloths, and health education.
The goals the Ministry will be advised to set include –
-
- To collaborate with Ministry of Water to ensure construction of at least one hand pump borewell in each endemic village within the next one year (May 2022) and scale up in two years (May 2023) to increase borewell in endemic villages to one borewell per 100 population.
- Administer correctly at least two rounds of correctly applied temephos in each endemic village during the next rainy season (April – September 2021) and scale up to administering four rounds in rainy season of 2022 and subsequently administering complete eight rounds during rainy season o 2023.
- Employ at least one community disease surveillance and notification officer in each endemic village whose role is to ensure all cases are reported within 24 hours. This employment and training should be completed, and officers deployed before beginning of rainy season by March 2022.
REFERENCES
1. Greenwood, B., Greenwood, A. & Bradley, A. Guinea worm infection in northern Nigeria: reflections on a disease approaching eradication. Trop. Med. Int. Heal. 22, 558–566 (2017).
2. Dracunculiasis (guinea-worm disease). https://www.who.int/news-room/fact-sheets/detail/dracunculiasis-(guinea-worm-disease).
3. Cairncross, S., Muller, R. & Zagaria, N. Dracunculiasis (guinea worm disease) and the eradication initiative. Clinical Microbiology Reviews vol. 15 223–246 (2002).
4. Cleveland, C. A. et al. A search for tiny dragons (Dracunculus medinensis third-stage larvae) in aquatic animals in Chad, Africa. Sci. Rep. 9, 1–7 (2019).
5. Nwoke, B. E. Behavioural aspects and their possible uses in the control of dracontiasis (guinea-worm) in Igwun river basin area of Imo State, Nigeria. Angew. Parasitol. 33, 205–210 (1992).
6. Microbial fact sheets – Guidelines for Drinking-Water Quality: Fourth Edition Incorporating the First Addendum – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK442360/.
7. Ruiz-Tiben, E. & Hopkins, D. R. Dracunculiasis (Guinea Worm Disease) Eradication. Advances in Parasitology (2006) doi:10.1016/S0065-308X(05)61007-X.
8. (No Title). https://www.cartercenter.org/resources/pdfs/news/features/guinea_worm/gw-maps-1986-2010.pdf.
9. Parenti, D. M. Dracunculiasis. in Medical Parasitology 58–62 (CRC Press, 2009). doi:10.1201/9781498713672-18.
10. Muller, R. Guinea worm disease: Epidemiology, control and treatment. Bull. World Health Organ. 57, 683–689 (1979).
11. Dracunculus. https://parasite.org.au/para-site/text/dracunculus-text.html.
12. Hopkins, D. R., Ruiz-Tiben, E., Eberhard, M. L., Roy, S. L. & Weiss, A. J. Progress Toward Global Eradication of Dracunculiasis, January 2016–June 2017. MMWR. Morb. Mortal. Wkly. Rep. 66, 1327–1331 (2017).
13. Prevention, C.-C. for D. C. and. CDC – Guinea Worm Disease – Epidemiology & Risk Factors. (2019).
14. Guagliardo, S. A. J. et al. Guinea worm in domestic dogs in chad: A description and analysis of surveillance data. PLoS Negl. Trop. Dis. 14, 1–17 (2020).
15. Richards, R. L. et al. Identifying correlates of Guinea worm (Dracunculus medinensis) infection in domestic dog populations. PLoS Negl. Trop. Dis. 14, e0008620 (2020).
16. WHO | Chemical control of copepods. WHO (2017).
17. Netshikweta, R. & Garira, W. A Multiscale Model for the World’s First Parasitic Disease Targeted for Eradication: Guinea Worm Disease. Comput. Math. Methods Med. 2017, (2017).
18. Prevention, C.-C. for D. C. and. CDC – Guinea Worm Disease – General Information – Frequently Asked Questions (FAQs). (2020).
19. Cairncross, S., Braide, E. I. & Bugri, S. Z. Community participation in the eradication of guinea worm disease. Acta Trop. 61, 121–136 (1996).
20. Eberhard, M. L. et al. Possible role of fish and frogs as paratenic hosts of Dracunculus medinensis, Chad. Emerg. Infect. Dis. 22, 1428–1430 (2016).








Post Comment