Gut Microbiota and Mental Health: Cause, Correlation, or Both?
Introduction
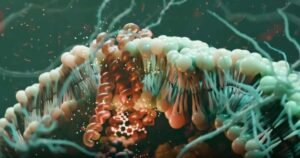
Over the past decade, scientists have uncovered a surprising connection between our gut and our brain. This link, often called the microbiota–gut–brain axis, shows that the trillions of microbes in our intestines may influence not just digestion, but also mood, stress, and even serious mental health conditions.
But here’s the big question: does the gut microbiota directly cause mental health disorders, simply correlate with them, or work in a two-way relationship? Understanding this could reshape how we approach treatments for depression, anxiety, PTSD, and schizophrenia.
What Is the Gut Microbiota?
The gut microbiota is the community of bacteria, fungi, and other tiny organisms that live in our digestive system. Think of it as a bustling ecosystem inside your intestines. These microbes don’t just help break down food—they also:
- Produce metabolites (small molecules that affect body functions).
- Interact with the immune system.
- Send signals to the nervous system, influencing the brain.
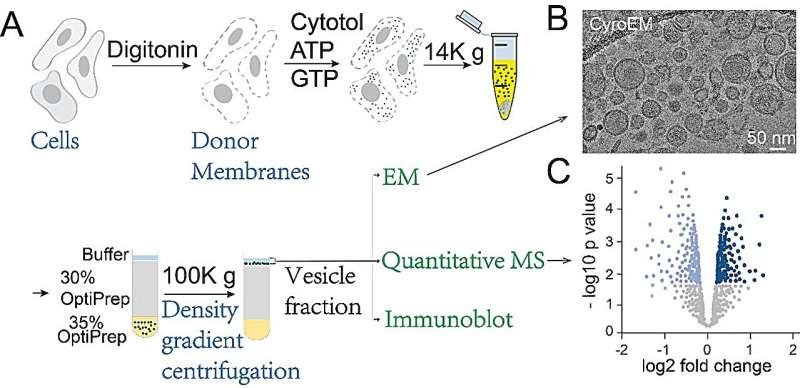
The Microbiota–Gut–Brain Axis Explained
This axis is a two-way communication system between the gut and the brain. Messages travel back and forth through:
- Neural pathways like the vagus nerve.
- Immune signals that trigger inflammation or healing.
- Metabolites such as short-chain fatty acids that impact mood and brain chemistry.
In short, your gut can “talk” to your brain—and your brain can also “talk” back to your gut.
Cause, Correlation, or Both?
1. Causative Role
Some studies show that changing gut microbes can directly alter mood and behavior. For example:
- Transferring gut bacteria from depressed individuals into animals often triggers depression-like symptoms in the animals.
- Probiotics and prebiotics (foods that feed good bacteria) sometimes reduce anxiety or improve mood.
This suggests the gut microbiota can play a causal role in mental health.
2. Correlative Role
On the other hand, many studies only show patterns. People with depression, anxiety, or schizophrenia often have different gut microbiota than healthy individuals. But this doesn’t prove one causes the other—it could simply be a correlation.
3. Bidirectional Role
Most researchers now believe the relationship is bidirectional. Stress and poor mental health can change gut bacteria, while unhealthy gut bacteria can worsen mental health. It’s a cycle that feeds into itself.
Why This Matters for Mental Health
If we can clearly distinguish cause from correlation, the benefits are huge:
- New treatments: Targeting gut microbes with diet, probiotics, or even fecal microbiota transplants.
- Personalized medicine: Using microbiome tests to predict who might respond best to certain therapies.
- Better prevention: Lifestyle choices (like diet and stress management) that nurture a healthy gut may lower mental health risks.
Current Challenges in Research
Despite exciting progress, several challenges remain:
- Most studies are small and limited to certain populations, making it hard to generalize results.
- It’s difficult to prove cause-and-effect in humans because so many factors (diet, stress, genetics) interact with gut microbes.
- Standardized methods are still evolving, so results vary between studies.
Conclusion
The gut microbiota is no longer just a curiosity—it may be a key player in mental health. While research is still untangling whether microbes cause, correlate, or mutually interact with mental illness, one thing is clear: the microbiota–gut–brain axis has the potential to transform mental health care.
Future therapies might not only treat symptoms but also re-balance the gut ecosystem to support long-term mental well-being.
👉 Stay tuned to advances in this field—what happens in your gut may shape the future of psychiatry.








Post Comment