Blog
acetate cross-feeding, antibiotic resistance, BacArena, biofilm metabolism, chronic UTI, COBRA Toolbox, context-specific modeling, D-mannose, E. coli virulence, Escherichia coli metabolism, female UTI, flux variability analysis, FPKM, gapseq, GEMs, genome-scale metabolic modeling, glycolysis in UTI, Human Urine Metabolome, Lactobacillus in UTI, MDR UTI, metabolic flux analysis, metabolic subsystems, metatranscriptomics, microbial community, microbial cross-feeding, microbial diversity, microbiome diagnostics, ornithine production, patient-specific models, PCA microbiome, personalized UTI treatment, precision medicine, probiotic therapy, Rank Math SEO, recurrent UTI, RNA sequencing, Shannon diversity, siderophores, systems biology, UPEC, urinary health, urinary metabolites, urinary microbiota, urinary tract infection, urine metabolome, uropathogenic E. coli, UTI microbiome, VFDB, women’s health
clinicalmicrobiology.org
0 Comments
Beyond E. coli: Why Your UTI is a Personalized Microbial Battle (And How Science is Mapping It)
For decades, urinary tract infections (UTIs) have been seen as a simple problem: bad bacteria (usually E. coli) invade, and antibiotics kick them out. But what if that’s only half the story?
A groundbreaking new study flips the script. Researchers didn’t just look at which bacteria were in the urine of 19 women with UTIs—they listened to what those bacteria were saying and doing. By combining gene activity tracking with advanced computer modeling, they discovered that UTIs are deeply personal, complex battles shaped by your unique mix of microbes and their real-time metabolic teamwork.
This isn’t just academic—it’s the future of fighting UTIs, especially as antibiotic resistance grows. Let’s break down what they found.
UTIs Aren’t a Solo Act: It’s a Microbial Community Affair
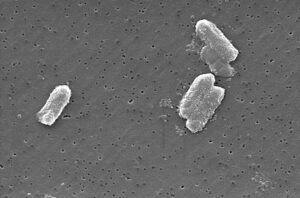
First, the researchers confirmed what recent science has been hinting at: your urinary tract isn’t sterile, even when you’re sick. The 19 patients didn’t just have E. coli. Their urine teemed with a diverse cast of characters, including bacteria typically found in the gut, mouth, and vagina.
Some key takeaways:
- Surprising Guests: Bacteria like Prevotella, Dialister, and Porphyromonas—often linked to other body sites—were active players in the UTI environment.
- The Lactobacillus Mystery: Perhaps most intriguingly, several patients had significant populations of Lactobacillus species—the “good” bacteria often associated with vaginal health. Their presence didn’t prevent the UTI, suggesting their role is more complex than simply being protective.
- Two Patient Types: The study essentially revealed two groups: those with a simple, E. coli-dominated infection, and those with a more complex “microbial neighborhood” that included diverse Lactobacillus species.
This diversity means that a one-size-fits-all antibiotic approach is increasingly outdated. Your UTI is as unique as your microbiome.
Listening to E. coli: What Its Genes Reveal About Its Attack Strategy
Since E. coli causes about 80% of UTIs, the researchers zoomed in on its activity. They mapped which genes were turned “on” (expressed) in each patient, revealing the bacteria’s real-time battle plan.
Here’s what E. coli was busy doing:
- Sticking Around: Genes for making “fimbrae” (tiny grappling hooks) were highly active, helping the bacteria cling to bladder walls.
- Stealing Iron: In the nutrient-poor urinary tract, E. coli ramped up genes for scavenging iron—a crucial element for its survival and growth.
- The Unknowns: A significant portion of the most active genes had no known function. This “dark matter” of bacterial genetics could hold clues to new virulence mechanisms or treatment targets.
Crucially, how E. coli behaved varied from patient to patient. Some strains were hyper-aggressive, while others seemed to be in a more dormant state. This personalization explains why infections can feel different and respond differently to treatment.
The Power of Metabolic Modeling: Simulating Your Personal UTI in a Computer
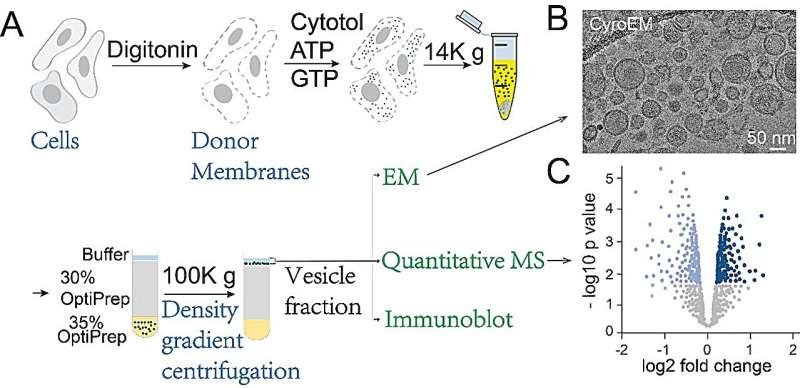
This is where the study gets truly innovative. The researchers didn’t stop at gene lists. They fed this gene activity data into sophisticated computer models called genome-scale metabolic models (GEMs).
Think of a GEM as a digital twin of a bacterium’s entire metabolic network—every chemical reaction it can perform. By constraining these models with the actual gene activity from each patient’s sample, they created a “context-specific” simulation of what the bacteria were metabolically capable of in that specific person, at that specific time.
The results were eye-opening:
- Metabolic Fingerprints: Each patient’s UTI community had a unique metabolic “fingerprint.” Some were focused on sugar breakdown, others on amino acid scavenging, and others on producing specific waste products.
- Lactobacillus Changes the Game: In patients with diverse Lactobacillus populations, the overall metabolic activity of the microbial community was lower. This suggests Lactobacillus might be subtly influencing or even suppressing the metabolism of the pathogens.
- Narrowing the Focus: When gene activity data was used to constrain the models, the range of possible metabolic reactions shrank dramatically. This means the models became much more biologically accurate, focusing only on the pathways the bacteria were actually using.
The Hidden Conversations: How Bacteria “Talk” Through Chemistry (Cross-Feeding)
Perhaps the most fascinating discovery was evidence of metabolic cross-feeding—a form of chemical teamwork (or exploitation) between different bacteria in your urinary tract.
The models showed:
- Lactobacillus as Supplier: Certain Lactobacillus species were producing metabolites like acetate (a short-chain fatty acid) and alpha-lactose.
- E. coli as Consumer: While direct consumption wasn’t always observed, E. coli and other pathogens were shown to be consuming similar metabolites. It’s highly plausible that the “good” bacteria are inadvertently feeding the “bad” ones.
- The Ornithine Trick: E. coli itself was producing ornithine, an amino acid that was then consumed by other community members. This could be a strategy to manipulate the environment to its own advantage.
This cross-feeding turns the UTI from a simple invasion into a complex ecosystem. Bacteria aren’t just fighting your body; they’re also negotiating, cooperating, and competing with each other.
What This Means for You: The Future of Personalized UTI Care
This research is a massive leap toward truly personalized medicine for UTIs. Here’s what it could mean:
- Better Diagnostics: Instead of just identifying E. coli, future tests could analyze the metabolic signature of your infection, revealing its unique vulnerabilities.
- Smarter Treatments: Treatments could target specific metabolic pathways that a patient’s unique bacterial community relies on, rather than using broad-spectrum antibiotics. For example, blocking a key nutrient exchange or cross-fed metabolite.
- Probiotic Precision: Understanding how Lactobacillus interacts metabolically with pathogens could lead to next-generation probiotics designed not just to add good bacteria, but to disrupt the harmful metabolic networks.
- Dietary Interventions: If certain foods fuel the pathogenic metabolism, dietary changes could become a powerful tool to prevent or manage UTIs.
The Bottom Line: Your UTI is More Complex (and Personal) Than You Think
This study shatters the old, simplistic view of UTIs. It’s not just E. coli vs. you. It’s a dynamic, personalized ecosystem of microbes, each with its own metabolic agenda, interacting with each other and your body in real-time.
While we’re not there yet, this research paves the way for a future where UTI treatment is tailored to your unique microbial fingerprint. The goal? To outsmart the infection by understanding its inner workings, moving beyond the blunt instrument of antibiotics to precise, effective, and personalized care.
If you suffer from recurrent UTIs, talk to your doctor about emerging research. The future of treatment is being written in the language of microbial metabolism—and it’s incredibly promising.








Post Comment