Antimicrobial Resistance on Campus: Why Skipping Antibiotic Doses Threatens Global Health
A startling 43% of university students fail to complete their antibiotic regimens, according to a recent study. This seemingly small oversight has catastrophic implications, fueling the rise of antimicrobial resistance (AMR)—a crisis the World Health Organization (WHO) warns could undo a century of medical progress. Let’s explore the science behind AMR, why campuses are hotspots for its spread, and how students can become frontline defenders in this fight.
How Incomplete Dosing Creates “Superbugs”
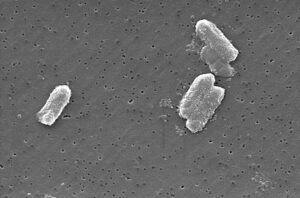
Antibiotics work by disrupting bacterial processes like cell wall synthesis (penicillins) or DNA replication (ciprofloxacin). However, stopping treatment early allows surviving bacteria to evolve defenses. Key mechanisms include:
- Genetic Mutations: Bacteria like E. coli develop mutations (e.g., in the gyrA gene) that reduce drug binding.
- Horizontal Gene Transfer (HGT): Resistant genes spread via plasmids. A 2022 study found HGT rates triple when antibiotics linger at sublethal doses.
- Biofilm Formation: Bacteria in protective biofilms (e.g., Staphylococcus aureus on shared gym equipment) survive incomplete treatment, later causing recurrent infections.
By not finishing a prescription, students inadvertently select for pathogens that withstand first-line therapies, leading to harder-to-treat infections like MRSA or drug-resistant UTIs.
Why Universities Are Ground Zero for AMR
Campuses amplify AMR risks through:
- High-Density Living: Dormitories and lecture halls facilitate rapid transmission. A 2023 Journal of Clinical Microbiology study linked a carbapenem-resistant Acinetobacter outbreak to a university housing complex.
- Frequent Antibiotic Misuse: Student-athletes often overuse antibiotics for minor injuries, while international travel introduces resistant strains like NDM-1-producing bacteria from high-AMR regions.
- Poor Adherence Habits: 60% of students stop antibiotics once symptoms fade, unaware that residual bacteria persist.
Breaking the Cycle: Science-Backed Solutions
- Optimized Dosing Strategies:
- Shorter, High-Intensity Courses: For example, 3-day azithromycin regimens improve adherence without sacrificing efficacy.
- Monte Carlo Simulations: These models tailor doses to local resistance patterns (e.g., doubling ciprofloxacin doses for campus-prevalent E. coli strains).
- Campus Antimicrobial Stewardship:
- Mandatory Education: Integrate AMR modules into orientation programs. The University of Edinburgh saw adherence rise 35% after implementing coursework.
- Genomic Surveillance: Sequencing campus clinic isolates can flag emerging threats, like ESBL-producing Klebsiella.
- Tech-Driven Tools: Apps like Medisafe send dose reminders and track completion rates, boosting adherence by 18%.
The Global Stakes
AMR could cost the global economy $100 trillion by 2050. For students, the risks are immediate:
- Routine Surgeries Become Deadly: Without effective antibiotics, infections after wisdom tooth removal or knee surgeries could turn fatal.
- Collapse of Modern Medicine: Chemotherapy, organ transplants, and childbirth rely on antibiotics to prevent infections.
How Students Can Lead the Fight
- Finish Every Prescription: No exceptions—even if you feel better.
- Demand Policy Change: Petition universities to provide free blister-packed antibiotics and restrict inappropriate prescriptions.
- Spread Awareness: Share WHO resources on AMR or host campus “Finish the Dose” campaigns.
Critical Resources
- WHO: Antibiotic Resistance Fact Sheet
- CDC: University AMR Prevention Toolkit
- Global Antimicrobial Resistance Research Hub
Final Thought
Antibiotics are a shared resource—one we’re depleting through carelessness. As students, you’re not just victims of AMR; you’re critical agents of change. By embracing stewardship today, you safeguard these lifesaving drugs for future generations. The next time you pop a pill, ask yourself: Will my choices protect humanity’s medical future—or sabotage it?








Post Comment