Harnessing Probiotics to Restore Microbiome Balance After Antibiotic Disruption
Restoring Microbiome Balance with Dual-Channel Probiotics
Antibiotics are life-saving medications, but they often disrupt the delicate balance of beneficial bacteria in our bodies, leading to conditions like intestinal and vaginal dysbiosis. A groundbreaking study explores how dual-channel probiotics can help restore this balance, offering new hope for those affected by antibiotic-induced microbiome disturbances.
In this article, we’ll break down the study’s findings, explain the mechanisms behind probiotic action, and discuss why this research matters for improving human health.
Understanding Dysbiosis
Dysbiosis refers to an imbalance in the microbial communities within the body, often caused by factors like antibiotic use, poor diet, or illness. This imbalance can lead to a range of health issues, including gastrointestinal problems, vaginal infections, and weakened immune function.
The study focuses on two key areas affected by dysbiosis: the intestines and the vagina, both of which play crucial roles in overall health. By addressing these areas simultaneously, researchers aim to develop more effective solutions for restoring microbiome balance.
The Study: Investigating Dual-Channel Probiotics
The study aimed to evaluate the effectiveness of dual-channel probiotics in correcting dysbiosis caused by antibiotics. Here’s how the researchers conducted their investigation:
Experimental Design
- Animal Models:
Mice were used as models to simulate antibiotic-induced dysbiosis. They were divided into four treatment groups:- PM Group: Saline (control).
- PA Group: Standard triple therapy (amoxicillin, clarithromycin, omeprazole).
- PL Group: Probiotic strain Lactobacillus reuteri NCU-15.
- PAL Group: Combination of triple therapy and L. reuteri NCU-15.
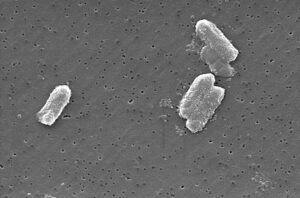
- Histopathological Analysis:
Tissue samples from the stomach, colon, and vagina were collected, fixed, and stained using H&E and Giemsa staining to assess microbial structure and inflammation levels under a microscope. - Quantitative PCR (qPCR):
qPCR was used to quantify microbial populations and evaluate the effectiveness of treatments in restoring balance.
Key Findings
- Probiotic Efficacy:
- The PL Group showed significant improvements in microbial diversity and reduced inflammation compared to the PM and PA groups.
- The PAL Group demonstrated the most robust recovery, highlighting the synergistic effect of combining probiotics with standard antibiotic therapy.
- Vaginal and Intestinal Health:
- Probiotics effectively restored Lactobacillus populations in the vagina, reducing symptoms of dysbiosis.
- In the intestines, probiotics helped rebuild beneficial bacterial communities, mitigating the harmful effects of antibiotics.
- Microbial Structure:
Giemsa staining revealed that probiotic-treated groups had healthier microbial structures in the stomach, indicating improved digestion and nutrient absorption.
Why This Matters
This research has significant implications for healthcare and microbiome science:
Addressing Antibiotic Side Effects
Antibiotics are essential for treating infections, but their impact on the microbiome can lead to long-term health issues. Probiotics offer a natural way to counteract these side effects, promoting faster recovery and better overall health.
Preventing Recurrent Infections
By restoring healthy microbial communities, probiotics can reduce the risk of recurrent infections, such as urinary tract infections (UTIs) and bacterial vaginosis (BV).
Advancing Personalized Medicine
The study highlights the potential of personalized probiotic therapies tailored to individual needs, paving the way for more targeted and effective treatments.
Recommendations for Future Research
While the findings are promising, further studies are needed to validate and expand upon these results:
Human Trials
Future research should focus on human trials to confirm the efficacy of dual-channel probiotics in real-world settings.
Long-Term Effects
Longitudinal studies are necessary to assess the long-term benefits of probiotic interventions and their impact on chronic conditions like inflammatory bowel disease (IBD).
Mechanistic Insights
More research is needed to understand the exact mechanisms by which probiotics interact with the host microbiome and immune system.
Looking Ahead
This study marks a significant step forward in understanding how probiotics can mitigate the negative effects of antibiotics. By leveraging the power of beneficial bacteria, we can improve outcomes for patients and reduce the burden of antibiotic-associated complications.
Collaboration between researchers, clinicians, and industry stakeholders will be crucial to translating these findings into practical applications.
Conclusion: Join the Microbiome Revolution
The microbiome plays a vital role in our health, and maintaining its balance is essential for preventing and managing a wide range of conditions. Probiotics offer a safe and effective way to restore this balance, especially after antibiotic use.
If you’re interested in learning more about the microbiome or want to support ongoing research, consider sharing this article with your network. Together, we can promote awareness and drive progress toward healthier lives.








Post Comment