Understanding and Combating Carbapenem-Resistant Enterobacterales in Bihar, India: A Comprehensive Study
Unpacking the Threat of Carbapenem-Resistant Enterobacterales
Carbapenem-resistant Enterobacterales (CRE) infections are a pressing global health concern due to their limited treatment options and high mortality rates. A recent study conducted at a tertiary care center in Bihar, India, sheds light on the alarming prevalence and resistance patterns of CRE in the region.
In this article, we’ll break down the findings of the study, explain the methods used to identify CRE, and discuss why these insights matter for public health.
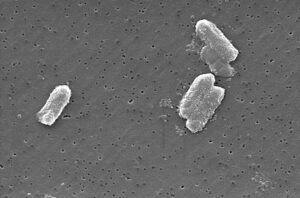
What Are Carbapenem-Resistant Enterobacterales?
Carbapenem-resistant Enterobacterales (CRE) are bacteria that have developed resistance to carbapenems—a class of powerful antibiotics often considered the “last line of defense” against severe infections. These bacteria can cause serious illnesses like pneumonia, urinary tract infections, and bloodstream infections.
CRE infections are particularly dangerous because they leave clinicians with few treatment options. Antibiotics like colistin and newer beta-lactam-beta-lactamase inhibitor combinations (BL-BLIs) are often the only choices, but even these are becoming less effective.
The Study: Investigating CRE in Bihar
The study aimed to determine the prevalence, phenotypic characteristics, and antibiotic resistance profiles of CRE isolates in Bihar, India. Here’s how the researchers approached the problem:
Study Design and Methods
- Sample Collection:
Researchers analyzed 3,421 Enterobacterales isolates collected from both inpatients and outpatients between July 2021 and July 2023. - Detection Techniques:
- Modified Carbapenem Inactivation Method (mCIM): Used to detect carbapenemase enzymes.
- EDTA-Modified Carbapenem Inactivation Method (eCIM): Specifically identified metallo-beta-lactamases (Class B carbapenemases).
- Combined Disc Tests: Classified CRE into different classes based on their resistance mechanisms.
- Antibiotic Susceptibility Testing:
Isolates were tested against a range of antibiotics, including third-generation cephalosporins, BL-BLIs, fluoroquinolones, and aminoglycosides.
Key Findings
- High Prevalence of CRE:
- 32.97% of all Enterobacterales isolates were carbapenem-resistant.
- Inpatients showed significantly higher resistance rates (47.74%) compared to outpatients (14.48%).
- Resistance Patterns:
- All CRE isolates were resistant to third-generation cephalosporins, BL-BLIs, and aztreonam.
- Resistance to fluoroquinolones, aminoglycosides, and other antibiotics was also widespread.
- Only one isolate showed resistance to colistin, highlighting its importance as a last-resort treatment.
- Dominance of Class B Carbapenemases:
- 70% of E. coli and 55% of Klebsiella pneumoniae isolates produced Class B carbapenemases.
- Co-expression of Class A and Class B carbapenemases was observed in 23% of E. coli and 36.2% of K. pneumoniae isolates.
Why This Matters
The findings from this study have significant implications for healthcare and public health policies:
Limited Treatment Options
With most CRE isolates resistant to multiple antibiotics, clinicians face challenges in selecting effective treatments. The emergence of colistin resistance—even in small numbers—raises concerns about future treatment failures.
Spread of Resistance
The high prevalence of CRE in hospital settings underscores the need for stricter infection control measures. Factors like overuse of antibiotics, poor hygiene practices, and inadequate surveillance contribute to the spread of resistant strains.
Global Health Threat
CRE infections are not just a local issue—they pose a global health threat. Without intervention, these bacteria could become endemic, making infections harder to treat and increasing healthcare costs.
Recommendations for Addressing CRE
The study authors propose several strategies to combat the rise of CRE:
Standardized Phenotypic Testing
Phenotypic tests like mCIM and eCIM are cost-effective and adaptable for resource-limited settings. They can guide therapy and enhance infection control efforts.
Improved Infection Control
Hospitals must enforce strict hand hygiene, surface decontamination, and patient isolation protocols. Routine screening for CRE colonization can help prevent outbreaks.
Antibiotic Stewardship
Promoting responsible antibiotic use is critical to slowing the development of resistance. Hospitals should develop antimicrobial policies based on local antibiograms.
Research and Development
The study highlights the urgent need for new antibiotics and diagnostic tools to address the growing threat of CRE.
Looking Ahead
While this study provides valuable insights, it also highlights gaps in our understanding of CRE. Future research should focus on genotypic characterization and long-term surveillance to monitor resistance trends.
Collaboration between healthcare facilities, policymakers, and researchers is essential to implement effective interventions and curb the spread of CRE.
Conclusion: Join the Fight Against CRE
Carbapenem-resistant Enterobacterales represent a significant challenge to modern medicine. By understanding their prevalence and resistance mechanisms, we can take steps to combat their spread.
If you’re passionate about public health or want to stay informed about the latest scientific breakthroughs, consider sharing this article with your network. Together, we can raise awareness and drive progress toward a healthier future.








Post Comment