Understanding the Role of Integrons in Antibiotic Resistance Among Burn Wound Infections
Unpacking the Role of Integrons in Antibiotic Resistance
Antibiotic resistance is a growing global health crisis, and one of its key drivers is the spread of genetic elements called integrons. These DNA segments allow bacteria to acquire and share resistance genes, making infections harder to treat. A recent study sheds light on the prevalence and impact of integrons in Acinetobacter baumannii, a notorious pathogen often found in burn wound infections.
In this article, we’ll break down what integrons are, their role in antibiotic resistance, and why understanding them is crucial for addressing multidrug-resistant (MDR) infections.
What Are Integrons?
Integrons are genetic structures that help bacteria adapt to antibiotics by capturing and expressing resistance genes. Think of them as “genetic toolkits” that bacteria use to survive in hostile environments like hospitals. They come in three main types—Class 1, Class 2, and Class 3—each with unique characteristics and roles.
- Class 1 integrons are the most common and often carry genes for resistance to multiple antibiotics.
- Class 2 integrons are less frequent but still contribute to resistance.
- Class 3 integrons are rare but emerging as a concern in some regions.
These integrons are particularly problematic in healthcare settings, where they spread rapidly among bacterial populations.
The Study: Investigating Integrons in Burn Wound Infections
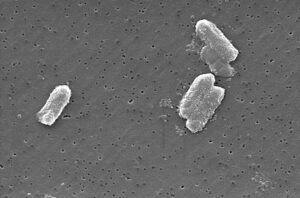
The study focused on Acinetobacter baumannii, a bacterium known for causing severe infections in burn patients. Researchers analyzed clinical isolates from burn wound infections to determine the prevalence of different integron classes and their association with antibiotic resistance.
Key Findings
- High Prevalence of Class 1 and Class 3 Integrons:
- 74% of isolates carried the intI1 gene (associated with Class 1 integrons).
- 45% of isolates had the intI3 gene (linked to Class 3 integrons).
- No isolates contained the intI2 gene (Class 2 integrons).
- Multidrug Resistance (MDR):
All isolates were multidrug-resistant, showing resistance to antibiotics like ciprofloxacin, ceftriaxone, and cefepime. Doxycycline was the most effective drug, but resistance rates were still alarmingly high at 88%. - Impact on Treatment:
The widespread presence of integrons highlights the misuse of broad-spectrum antibiotics, which accelerates resistance. This trend makes infections harder to manage and increases mortality risks for burn patients.
Why This Matters
Understanding the role of integrons is critical for developing strategies to combat antibiotic resistance. Here’s why:
Spread of Resistance Genes
Integrons act as vehicles for spreading resistance genes across bacterial species. For example, the aadA2 and dfrA12 gene cassettes found in many isolates confer resistance to antibiotics like streptomycin and trimethoprim.
Challenges in Burn Care
Burn patients are especially vulnerable to infections due to compromised skin barriers and weakened immune systems. When integrons enable bacteria like A. baumannii to resist treatment, it prolongs recovery times and increases healthcare costs.
Implications for Public Health
The study underscores the urgent need for better antibiotic stewardship and infection control measures. Without intervention, the rise of integron-mediated resistance could render current treatments ineffective.
How Can We Address the Problem?
While the findings are concerning, they also offer actionable insights:
Improved Antibiotic Policies
Hospitals must adopt stricter guidelines for antibiotic use, avoiding unnecessary prescriptions of broad-spectrum drugs. Tailored treatments based on susceptibility testing can reduce selective pressure on bacteria.
Enhanced Surveillance
Regular monitoring of integron prevalence and resistance patterns can help identify emerging threats early. Molecular techniques like PCR can detect integrons quickly and accurately.
Research and Innovation
Developing new antibiotics and alternative therapies, such as phage therapy or efflux pump inhibitors, is essential. Additionally, vaccines targeting resistant pathogens could provide long-term solutions.
Looking Ahead
This research highlights the complex interplay between genetic factors and antibiotic resistance. By focusing on integrons, scientists can gain deeper insights into how bacteria evolve and adapt. Future studies should explore the mechanisms behind integron mobility and their interactions with other genetic elements.
For now, the message is clear: addressing antibiotic resistance requires a multifaceted approach involving healthcare providers, researchers, and policymakers. Together, we can slow the spread of MDR bacteria and protect vulnerable populations like burn patients.
Conclusion: Join the Fight Against Antibiotic Resistance
Antibiotic resistance isn’t just a medical issue—it’s a global challenge that demands collective action. Understanding the role of integrons in infections like those caused by Acinetobacter baumannii is a vital step toward finding solutions.
If you’re passionate about public health or want to stay informed about the latest scientific breakthroughs, consider sharing this article with your network. Together, we can raise awareness and drive progress toward a healthier future.








Post Comment