Curved Gram-Negative Rods: Campylobacter and Helicobacter Explained

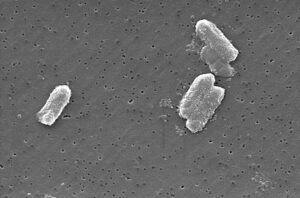
Certain bacteria, like Campylobacter and Helicobacter, have a distinctive curved or spiral shape and are important pathogens that cause gastrointestinal illnesses.
This breakdown explains their features, how they are diagnosed, and how infections are managed.
Campylobacter
What is it?
- A gram-negative, spiral-shaped bacterium that thrives in low-oxygen environments (microaerophilic).
- Known for its corkscrew motion, which helps it invade tissues.
How do people get it?
- Mostly from eating undercooked poultry, unpasteurized milk, or drinking contaminated water.
- It’s a leading cause of foodborne illness worldwide.
What does it cause?
- Symptoms include diarrhea (sometimes bloody), abdominal cramps, fever, nausea, and fatigue.
- Rarely, it can trigger Guillain-Barré Syndrome, a condition that affects the nerves.
How is it diagnosed?
- Sample Collection: Stool is the preferred sample.
- Culture Media: Grown on selective media like Columbia blood agar under microaerophilic conditions.
- Growth Conditions: Requires 42°C incubation to mimic avian body temperature.
- Additional Tests: Oxidase-positive and catalase-positive tests help confirm identification.
How is it treated?
- Supportive care with oral rehydration is usually sufficient for mild cases.
- Antibiotics like azithromycin or ciprofloxacin are reserved for severe or prolonged infections.
Helicobacter
What is it?
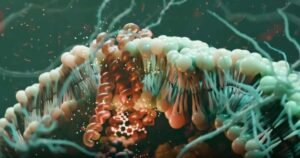
- A gram-negative, spiral bacterium that lives in the stomach lining.
- Produces urease, an enzyme that neutralizes stomach acid, allowing it to survive in a harsh acidic environment.

How do people get it?
- Spread through contaminated water, food, or close contact with infected individuals.
What does it cause?
- Long-term infections can lead to chronic gastritis, peptic ulcers, and even gastric cancer.
How is it diagnosed?
- Sample Collection: Gastric biopsy during endoscopy is the gold standard.
- Culture Media: Grown on enriched media like Skirrow’s agar or Columbia agar with 5-10% sheep blood under microaerophilic conditions.
- Biochemical Tests:
- Urease activity test: Rapid detection using biopsy material.
- Catalase and oxidase positive.
- Non-invasive Tests:
- Urea breath test: Detects urease activity indirectly.
- Stool antigen test for active infection.
How is it treated?
- Triple therapy:
- Proton pump inhibitor (e.g., omeprazole) to reduce stomach acid.
- Antibiotics (e.g., clarithromycin and amoxicillin or metronidazole) to eradicate bacteria.
- Bismuth-containing compounds to protect the stomach lining and enhance bacterial clearance.
Why Does It Matter?
Understanding these bacteria helps us appreciate how infections are connected to food safety and hygiene. With rising antibiotic resistance, proper diagnosis and judicious treatment are critical.
Questions to Test Your Knowledge:
- Which culture media and conditions are required for growing Campylobacter jejuni in the lab?
- How does Helicobacter pylori survive the acidic environment of the stomach?
- What are two complications caused by H. pylori infection?
- What are the steps involved in performing a stool culture for C. jejuni?
- How do the components of triple therapy for H. pylori work together to treat the infection?
By learning the detailed diagnostics and treatments, we can better understand how these bacteria affect human health and how to control their spread.








Post Comment