One Health: A Global Approach to Tackling Antimicrobial Resistance in Low- and Middle-Income Countries
One Health: A Global Approach to Tackling Antimicrobial Resistance in Low- and Middle-Income Countries
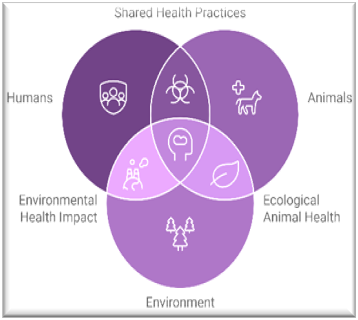
In a world where humans, animals, and the environment are inextricably linked, the concept of “One Health” has never been more relevant. One Health, a collaborative, multisectoral, and transdisciplinary approach, seeks to achieve optimal health outcomes by recognizing the interconnection between people, animals, plants, and their shared environment. Among the many pressing global health challenges, antimicrobial resistance (AMR) stands out as a crisis that requires the One Health approach to address effectively.
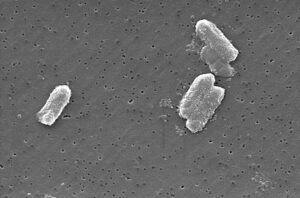
For low- and middle-income countries (LMICs), the stakes are especially high. AMR—the ability of microbes to resist the effects of drugs that once killed them—threatens to reverse decades of medical progress, undermining the fight against infectious diseases. Tackling AMR in LMICs requires a nuanced understanding of how human health, animal health, and environmental health intersect.
The Challenge of AMR in LMICs

LMICs bear a disproportionate burden of infectious diseases, and the spread of AMR compounds this challenge. Several factors contribute to the growing AMR crisis in these regions:
- Inappropriate Use of Antimicrobials: Antibiotics are often available over the counter without prescription, leading to misuse and overuse in both human medicine and animal husbandry. In many LMICs, antibiotics are even used as growth promoters in livestock.
- Weak Healthcare Systems: Limited access to diagnostics means that healthcare providers often prescribe antibiotics empirically, rather than based on laboratory evidence.
- Poor Sanitation and Hygiene: Inadequate wastewater treatment allows antibiotic residues and resistant bacteria from human and animal waste to contaminate water sources and agricultural fields.
- Global Trade and Travel: Resistant pathogens can easily spread across borders through human migration, trade in livestock, and agricultural products.
Why One Health Matters

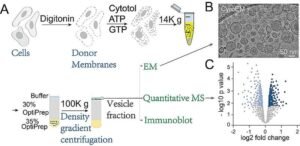
The One Health approach acknowledges that the health of humans, animals, and ecosystems are deeply interconnected. A siloed response to AMR—focusing solely on human health, for example—ignores the vast reservoirs of resistance genes in animals and the environment. Here’s how One Health can make a difference:
- Human Health: Strengthening stewardship programs in healthcare facilities and improving access to diagnostics can help reduce unnecessary antibiotic use.
- Animal Health: Regulating veterinary use of antibiotics, phasing out their use as growth promoters, and encouraging vaccination in livestock can minimize infections and the need for antibiotics.
- Environmental Health: Investing in wastewater treatment facilities and enforcing regulations to limit pharmaceutical and agricultural runoff can curb the environmental dissemination of resistant bacteria and genes.
The LMIC Perspective
Adopting the One Health approach in LMICs comes with unique challenges and opportunities:
Challenges:
- Resource Limitations: Implementing coordinated programs across human, animal, and environmental health sectors can be resource-intensive.
- Policy Gaps: Many LMICs lack robust policies to regulate antibiotic use and environmental contamination.
- Data Scarcity: Surveillance systems for tracking AMR are underdeveloped in most LMICs, limiting the ability to measure progress.
Opportunities:
- Community Engagement: Culturally appropriate education campaigns can empower communities to use antibiotics responsibly.
- Global Partnerships: International organizations and high-income countries can provide technical and financial support for One Health initiatives.
- Innovation: LMICs can leapfrog traditional approaches by adopting low-cost, scalable technologies for AMR detection and monitoring.
Moving Forward: A Call to Action
The fight against AMR is a shared responsibility that transcends borders. For LMICs, integrating One Health principles into national and regional strategies is essential. Here are some actionable steps:
- Strengthen Surveillance: Establish and expand AMR surveillance networks that include data from human, animal, and environmental sources.
- Build Capacity: Train healthcare workers, veterinarians, and environmental scientists in antimicrobial stewardship and One Health practices.
- Foster Collaboration: Encourage partnerships between governments, NGOs, academic institutions, and the private sector to share knowledge and resources.
- Promote Policy and Legislation: Advocate for policies that regulate antibiotic use in humans and animals, as well as environmental protections against contamination.
A Shared Future
The One Health approach is not just a theoretical framework—it is a practical necessity for addressing AMR in LMICs. By breaking down silos and fostering collaboration across disciplines, we can build resilient systems that safeguard human health, protect animal populations, and preserve environmental integrity. In this shared ecosystem, our actions today will determine the health of generations to come.
Together, through the lens of One Health, we can tackle the AMR crisis and create a healthier, more sustainable future for all.
Further Reading
- World Health Organization (WHO) – Antimicrobial Resistance
- Food and Agriculture Organization (FAO) – Tackling AMR in Agriculture
- Centers for Disease Control and Prevention (CDC) – One Health Approach to AMR
- O’Neill Report on Antimicrobial Resistance (2016)
- United Nations Environment Programme (UNEP) – Environmental Dimensions of AMR:
- ReAct – Action on Antibiotic Resistance








Post Comment